38
Poisoning
Craig Smollin, MD
Kent R. Olson, MD
INITIAL EVALUATION: POISONING OR OVERDOSE
Patients with drug overdoses or poisoning may initially have no symptoms or they may have varying degrees of overt intoxication. The asymptomatic patient may have been exposed to or may have ingested a lethal dose, but not yet exhibit any manifestations of toxicity. It is important to (1) quickly assess the potential danger, (2) consider gut and skin decontamination to prevent absorption, (3) treat complications if they occur, and (4) observe the asymptomatic patient for an appropriate interval.
 Assess the Danger
Assess the Danger
If the drug or poison is known, its danger can be assessed by consulting a text or computerized information resource or by calling a regional poison control center. (In the United States, dialing 1-800-222-1222 will direct the call to the regional poison control center.) Assessment will usually take into account the dose ingested; the time since ingestion; the presence of any symptoms or clinical signs; preexisting cardiac, respiratory, kidney, or liver disease; and, occasionally, specific serum drug or toxin levels. Be aware that the history given by the patient or family may be incomplete or unreliable.
IMMEDIATE 24-HOUR TOXICOLOGY CONSULTATION
Call your regional poison control center
U.S. toll-free 1-800-222-1222
 Observe the Patient
Observe the Patient
Asymptomatic or mildly symptomatic patients should be observed for at least 4–6 hours. Longer observation is indicated if the ingested substance is a sustained-release preparation or is known to slow gastrointestinal motility (eg, opioids, anticholinergics, aspirin) or may cause a delayed onset of symptoms (eg, acetaminophen, colchicine, hepatotoxic mushrooms). After that time, the patient may be discharged if no symptoms have developed. Before discharge, psychiatric evaluation should be performed to assess suicide risk. Intentional ingestions in adolescents should raise the possibility of unwanted pregnancy or sexual abuse.
THE SYMPTOMATIC PATIENT
In symptomatic patients, treatment of life-threatening complications takes precedence over in-depth diagnostic evaluation. Patients with mild symptoms may deteriorate rapidly, which is why all potentially significant exposures should be observed in an acute care facility. The following complications may occur, depending on the type of poisoning.
COMA
 Assessment & Complications
Assessment & Complications
Coma is commonly associated with ingestion of large doses of antihistamines (eg, diphenhydramine), benzodiazepines and other sedative-hypnotic drugs, ethanol, opioids, antipsychotic drugs, or antidepressants. The most common cause of death in comatose patients is respiratory failure, which may occur abruptly. Pulmonary aspiration of gastric contents may also occur, especially in victims who are deeply obtunded or convulsing. Hypoxia and hypoventilation may cause or aggravate hypotension, arrhythmias, and seizures. Thus, protection of the airway and assisted ventilation are the most important treatment measures for any poisoned patient.
 Treatment
Treatment
A. Emergency Management
The initial emergency management of coma can be remembered by the mnemonic ABCD, for Airway, Breathing, Circulation, and Drugs (dextrose, thiamine, and naloxone or flumazenil), respectively.
1. Airway—Establish a patent airway by positioning, suction, or insertion of an artificial nasal or oropharyngeal airway. If the patient is deeply comatose or if airway reflexes are depressed, perform endotracheal intubation. These airway interventions may not be necessary if the patient is intoxicated by an opioid or a benzodiazepine and responds to intravenous naloxone or flumazenil.
2. Breathing—Clinically assess the quality and depth of respiration and provide assistance, if necessary, with a bag-valve-mask device or mechanical ventilator. Administer supplemental oxygen, if needed. The arterial or venous blood CO2 tension is useful in determining the adequacy of ventilation. The arterial blood PO2 determination may reveal hypoxemia, which may be caused by respiratory depression, bronchospasm, pulmonary aspiration, or noncardiogenic pulmonary edema. Pulse oximetry provides an assessment of oxygenation, but is not reliable in patients with methemoglobinemia or carbon monoxide poisoning, unless a pulse oximetry device capable of detecting these forms of hemoglobin is used.
3. Circulation—Measure the pulse and blood pressure and estimate tissue perfusion (eg, by measurement of urinary output, skin signs, arterial blood pH). Place the patient on continuous ECG monitoring. Insert an intravenous line, and draw blood for glucose, electrolytes, serum creatinine and liver tests, and possible quantitative toxicologic testing.
4. Drugs—
a. Dextrose and thiamine—Unless promptly treated, severe hypoglycemia can cause irreversible brain damage. Therefore, in all obtunded, comatose or convulsing patients, give 50% dextrose, 50–100 mL by intravenous bolus, unless a rapid point-of-care blood sugar test rules out hypoglycemia. In alcoholic or very malnourished patients who may have marginal thiamine stores, give thiamine, 100 mg intramuscularly or in the intravenous fluids.
b. Opioid antagonists—Naloxone, 0.4–2 mg intravenously or 2–4 mg by intranasal spray, may reverse opioid-induced respiratory depression and coma. It is often given empirically to any comatose patient with depressed respirations. If opioid overdose is strongly suspected, give additional doses of naloxone (up to 5–10 mg may be required to reverse the effects of potent opioids). Note: Naloxone has a shorter duration of action (2–3 hours) than most common opioids; repeated doses may be required, and continuous observation for at least 3–4 hours after the last dose is mandatory.
c. Flumazenil—Flumazenil, 0.2–0.5 mg intravenously, repeated as needed up to a maximum of 3 mg, may reverse benzodiazepine-induced coma. Caution: In most circumstances, use of flumazenil is not advised as the potential risks outweigh its benefits. Flumazenil should not be given if the patient has coingested a potential convulsant drug, is a user of high-dose benzodiazepines, or has a seizure disorder because its use in these circumstances may precipitate seizures. Note: Flumazenil has a short duration of effect (2–3 hours), and resedation requiring additional doses may occur.
HYPOTHERMIA
 Assessment & Complications
Assessment & Complications
Hypothermia commonly accompanies coma due to opioids, ethanol, hypoglycemic agents, phenothiazines, barbiturates, benzodiazepines, and other sedative-hypnotics and central nervous system depressants. Hypothermic patients may have a barely perceptible pulse and blood pressure. Hypothermia may cause or aggravate hypotension, which will not reverse until the temperature is normalized.
 Treatment
Treatment
Treatment of hypothermia is discussed in Chapter 37. Gradual rewarming is preferred unless the patient is in cardiac arrest.
HYPOTENSION
 Assessment & Complications
Assessment & Complications
Hypotension may be due to poisoning by many different drugs, including antihypertensives, beta-blockers, calcium channel blockers, disulfiram (ethanol interaction), iron, trazodone, quetiapine, and other antipsychotic agents and antidepressants. Poisons causing hypotension include cyanide, carbon monoxide, hydrogen sulfide, aluminum or zinc phosphide, arsenic, and certain mushrooms.
Hypotension in the poisoned or drug-overdosed patient may be caused by venous or arteriolar vasodilation, hypovolemia, depressed cardiac contractility, or a combination of these effects.
 Treatment
Treatment
Most hypotensive poisoned patients respond to empiric treatment with repeated 200 mL intravenous boluses of 0.9% saline or other isotonic crystalloid up to a total of 1–2 L; much larger amounts may be needed if the victim is profoundly volume depleted (eg, as with massive diarrhea due to Amanita phalloides mushroom poisoning). Monitoring the central venous pressure (CVP) can help determine whether further fluid therapy is needed. Consider bedside cardiac ultrasound or pulmonary artery catheterization (or both) to assess CVP. If fluid therapy is not successful after adequate volume replacement, give dopamine or norepinephrine by intravenous infusion.
Hypotension caused by certain toxins may respond to specific treatment. For hypotension caused by overdoses of tricyclic antidepressants or other sodium channel blockers, administer sodium bicarbonate, 50–100 mEq by intravenous bolus injection. Norepinephrine 4–8 mcg/min by intravenous infusion is more effective than dopamine in some patients with overdoses of tricyclic antidepressants or of drugs with predominantly vasodilating effects. For beta-blocker overdose, glucagon (5–10 mg intravenously) may be of value. For calcium channel blocker overdose, administer calcium chloride, 1–2 g intravenously (repeated doses may be necessary; doses of 5–10 g and more have been given in some cases). High-dose insulin (0.5–1 unit/kg/h intravenously) euglycemic therapy may also be used (see the sections Beta-Adrenergic Blockers and Calcium Channel Blockers, below). Intralipid 20% lipid emulsion has been reported to improve hemodynamics in some cases of intoxication by highly lipid-soluble drugs such as bupivacaine, bupropion, clomipramine, and verapamil. Intravenous methylene blue and extracorporeal membrane oxygenation (ECMO) have been employed in a few refractory cases; ECMO may offer temporary hemodynamic stabilization while the offending drug is eliminated.
Chudow M et al. A case of severe, refractory hypotension after amlodipine overdose. Cardiovasc Toxicol. 2018 Apr;18(2):192–7. [PMID: 28688059]
Nafea OE et al. Comparative effectiveness of methylene blue versus intravenous lipid emulsion in a rodent model of amlodipine toxicity. Clin Toxicol (Phila). 2019 Sep;57(9):784–9. [PMID: 30729824]
Weiner L et al. Clinical utility of venoarterial-extracorporeal membrane oxygenation (VA-ECMO) in patients with drug-induced cardiogenic shock: a retrospective study of the Extracorporeal Life Support Organizations’ ECMO case registry. Clin Toxicol (Phila). 2020 Jul;58(7):705–10.] [PMID: 31617764]
HYPERTENSION
 Assessment & Complications
Assessment & Complications
Hypertension may be due to poisoning with amphetamines and synthetic stimulants, anticholinergics, cocaine, performance-enhancing products (eg, containing caffeine, phenylephrine, ephedrine, or yohimbine), monoamine oxidase (MAO) inhibitors, and other drugs.
Severe hypertension (eg, diastolic blood pressure greater than 105–110 mm Hg in a person who does not have chronic hypertension) can result in acute intracranial hemorrhage, myocardial infarction, or aortic dissection.
 Treatment
Treatment
Treat hypertension if the patient is symptomatic or if the diastolic pressure is higher than 105–110 mm Hg—especially if there is no prior history of hypertension.
Hypertensive patients who are agitated or anxious may benefit from a sedative (such as lorazepam, 2–3 mg intravenously) or an antipsychotic drug (eg, haloperidol or olanzapine). For persistent hypertension, administer phentolamine, 2–5 mg intravenously, or nitroprusside sodium, 0.25–8 mcg/kg/min intravenously. If excessive tachycardia is present, add esmolol, 25–100 mcg/kg/min intravenously, or labetalol, 0.2–0.3 mg/kg intravenously. Caution: Do not give beta-blockers alone, since doing so may paradoxically worsen hypertension in some cases as a result of unopposed alpha-adrenergic stimulation.
ARRHYTHMIAS
 Assessment & Complications
Assessment & Complications
Arrhythmias may occur with a variety of drugs or toxins (Table 38–1). They may also occur as a result of hypoxia, metabolic acidosis, or electrolyte imbalance (eg, hyperkalemia, hypokalemia, hypomagnesemia, or hypocalcemia), or following exposure to chlorinated solvents or chloral hydrate overdose. Atypical ventricular tachycardia (torsades de pointes) is often associated with drugs that prolong the QT interval.
Table 38–1. Common toxins or drugs causing arrhythmias.1

 Treatment
Treatment
Hypoxia or electrolyte imbalance should be sought and treated. If ventricular arrhythmias persist, administer lidocaine or amiodarone at usual antiarrhythmic doses. Note: Wide QRS complex tachycardia in the setting of tricyclic antidepressant overdose (or diphenhydramine or class Ia antiarrhythmic drugs) should be treated with sodium bicarbonate, 50–100 mEq intravenously by bolus infusion. Caution: In such cases, avoid class Ia antiarrhythmic agents (eg, procainamide, disopyramide) and amiodarone, which may aggravate arrhythmias caused by tricyclic antidepressants. Torsades de pointes associated with prolonged QT interval may respond to intravenous magnesium (2 g intravenously over 2 minutes) or overdrive pacing. Treat digitalis-induced arrhythmias with digoxin-specific antibodies.
For tachyarrhythmias induced by chlorinated solvents, chloral hydrate, Freons, or sympathomimetic agents, use propranolol or esmolol (see doses given above in Hypertension section).
Shakeer SK et al. Chloral hydrate overdose survived after cardiac arrest with excellent response to intravenous β-blocker. Oman Med J. 2019 May;34(3):244–8. [PMID: 31110633]
SEIZURES
 Assessment & Complications
Assessment & Complications
Seizures may be caused by many poisons and drugs, including amphetamines, antidepressants (especially tricyclic antidepressants, bupropion, and venlafaxine), antihistamines (especially diphenhydramine), antipsychotics, camphor, synthetic cannabinoids and cathinones, cocaine, isoniazid (INH), chlorinated insecticides, piperazines, tramadol, and theophylline. The onset of seizures may be delayed for up to 18–24 hours after extended-released bupropion overdose.
Seizures may also be caused by hypoxia, hypoglycemia, hypocalcemia, hyponatremia, withdrawal from alcohol or sedative-hypnotics, head trauma, central nervous system infection, or idiopathic epilepsy.
Prolonged or repeated seizures may lead to hypoxia, metabolic acidosis, hyperthermia, and rhabdomyolysis.
 Treatment
Treatment
Administer lorazepam, 2–3 mg, or diazepam, 5–10 mg, intravenously, or—if intravenous access is not immediately available—midazolam, 5–10 mg intramuscularly. If convulsions continue, administer phenobarbital, 15–20 mg/kg slowly intravenously over no less than 30 minutes. (For drug-induced seizures, phenobarbital is preferred over phenytoin or levetiracetam.) Propofol infusion has also been reported effective for some resistant drug-induced seizures.
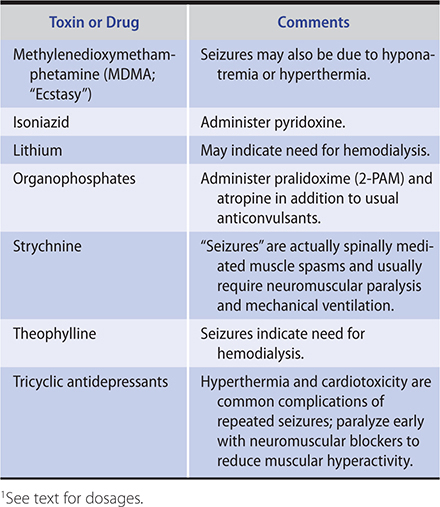
Seizures due to a few drugs and toxins may require antidotes or other specific therapies (as listed in Table 38–2).
Table 38–2. Seizures related to toxins or drugs requiring special consideration.1
Park HR et al. Endosulfan-induced prolonged super-refractory status epilepticus. J Epilepsy Res. 2018 Dec 31;8(2):93–6. [PMID: 30809504]
HYPERTHERMIA
 Assessment & Complications
Assessment & Complications
Hyperthermia may be associated with poisoning by amphetamines and other synthetic stimulants (cathinones, piperazines), atropine and other anticholinergic drugs, cocaine, salicylates, strychnine, 2,4-dinitrophenol, tricyclic antidepressants, and various other medications. Overdoses of serotonin reuptake inhibitors (eg, fluoxetine, paroxetine, sertraline) or their use in a patient taking an MAO inhibitor may cause agitation, hyperactivity, myoclonus, and hyperthermia (“serotonin syndrome”). Antipsychotic agents can cause rigidity and hyperthermia (neuroleptic malignant syndrome [NMS]). (See Chapter 25.) Malignant hyperthermia is a rare disorder associated with general anesthetic agents.
Hyperthermia is a rapidly life-threatening complication. Severe hyperthermia (temperature higher than 40–41°C) can rapidly cause brain damage and multiorgan failure, including rhabdomyolysis, acute kidney injury, and coagulopathy (see Chapter 37).
 Treatment
Treatment
Treat hyperthermia aggressively by removing the patient’s clothing, spraying the skin with tepid water, and high-volume fanning. Alternatively, the patient can be placed in an ice water bath (not simply applying ice to selected surfaces). If external cooling is not rapidly effective, as shown by a normal rectal temperature within 30–40 minutes, or if there is significant muscle rigidity or hyperactivity, induce neuromuscular paralysis with a nondepolarizing neuromuscular blocker (eg, rocuronium, vecuronium). Once paralyzed, the patient must be intubated and mechanically ventilated and sedated. While the patient is paralyzed, the absence of visible muscular convulsive movements may give the false impression that brain seizure activity has ceased; bedside electroencephalography may be useful in recognizing continued nonconvulsive seizures.
Dantrolene (2–5 mg/kg intravenously) may be effective for hyperthermia associated with muscle rigidity that does not respond to neuromuscular blockade (ie, malignant hyperthermia). Bromocriptine, 2.5–7.5 mg orally daily, has been recommended for neuroleptic malignant syndrome. Cyproheptadine, 4 mg orally every hour for three or four doses, or chlorpromazine, 25 mg intravenously or 50 mg intramuscularly, has been used to treat serotonin syndrome.
Kopec KT et al. Dinitrophenol (DNP) fatality associated with a falsely elevated salicylate level: a case report with verification of laboratory cross reactivity. J Med Toxicol. 2018 Dec;14(4):323–6. [PMID: 30051204]
Tormoehlen LM et al. Neuroleptic malignant syndrome and serotonin syndrome. Handb Clin Neurol. 2018;157:663–75. [PMID: 30459031]
Van Schoor J et al. Dantrolene is not the answer to 2,4-dinitrophenol poisoning: more heated debate. BMJ Case Rep. 2018 Dec 19;11(1):e225323. [PMID: 30573533]
ANTIDOTES & OTHER TREATMENT
ANTIDOTES
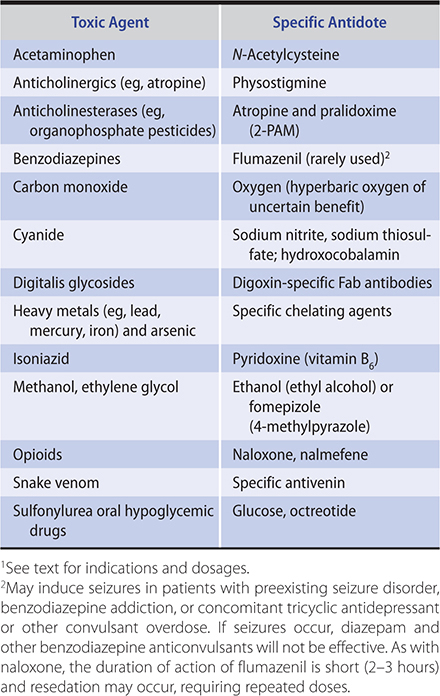
Give an antidote (if available) when there is reasonable certainty of a specific diagnosis (Table 38–3). Be aware that some antidotes themselves may have serious side effects. The indications and dosages for specific antidotes are discussed in the respective sections for specific toxins.
Table 38–3. Some toxic agents for which there are specific antidotes.1
Dzeshka MS et al. Direct oral anticoagulant reversal: how, when and issues faced. Expert Rev Hematol. 2017 Nov;10(11):1005–22. [PMID: 28901221]
Schwenk M. Chemical warfare agents. Classes and targets. Toxicol Lett. 2018 Sep 1;293:253–63. [PMID: 29197625]
DECONTAMINATION OF THE SKIN
Corrosive agents rapidly injure the skin and eyes and must be removed immediately. In addition, many toxins are readily absorbed through the skin, and systemic absorption can be prevented only by rapid action.
Wash the affected areas with copious quantities of lukewarm water or saline, taking care to limit exposure to health care providers. Wash carefully behind the ears, under the nails, and in skin folds. For oily substances (eg, pesticides), wash the skin at least twice with plain soap and shampoo the hair. Specific decontaminating solutions or solvents (eg, alcohol) are rarely indicated and in some cases may paradoxically enhance absorption. For exposure to chemical warfare poisons such as nerve agents or vesicants, some authorities recommend use of a dilute hypochlorite solution (household bleach diluted 1:10 with water), but not in the eyes.
DECONTAMINATION OF THE EYES
Act quickly to prevent serious damage. Flush the eyes with copious amounts of saline or water. (If available, instill local anesthetic drops in the eye before beginning irrigation.) Remove contact lenses if present. Lift the tarsal conjunctiva to look for undissolved particles and to facilitate irrigation. Continue irrigation for 15 minutes or until each eye has been irrigated with at least 1 L of solution. If the toxin is an acid or a base, check the pH of the tears after irrigation, and continue irrigation until the pH is between 6 and 8. An amphoteric decontamination solution (Diphoterine, Prevor) is used in some countries for treatment of alkali injuries to the eye.
After irrigation is complete, perform a careful examination of the eye, using fluorescein and a slit lamp or Wood lamp to identify areas of corneal injury. Patients with serious conjunctival or corneal injury should be immediately referred to an ophthalmologist.
GASTROINTESTINAL DECONTAMINATION
Removal of ingested poisons by induced emesis or gastric lavage was a routine part of emergency treatment for decades. However, prospective randomized studies have failed to demonstrate improved clinical outcome after gastric emptying. For small or moderate ingestions of most substances, toxicologists often recommend oral activated charcoal alone without prior gastric emptying; in some cases, when the interval after ingestion has been more than 1–2 hours and the ingestant is non–life-threatening, even charcoal is withheld (eg, if the estimated benefit is outweighed by the potential risk of pulmonary aspiration of charcoal). Exceptions are large ingestions of anticholinergic compounds and salicylates, which often delay gastric emptying, and ingestion of sustained-release or enteric-coated tablets, which may remain intact for several hours. In these cases, delayed gut decontamination may be indicated.
Gastric emptying is not generally used for ingestion of corrosive agents or petroleum distillates, because further esophageal injury or pulmonary aspiration may result. However, in certain cases, removal of the toxin may be more important than concern over possible complications. Consult a medical toxicologist or regional poison control center (1-800-222-1222) for advice.
A. Activated Charcoal
Activated charcoal effectively adsorbs almost all drugs and poisons. Poorly adsorbed substances include iron, lithium, potassium, sodium, mineral acids, and alcohols.
1. Indications—Activated charcoal can be used for prompt adsorption of drugs or toxins in the stomach and intestine. However, evidence of benefit in clinical studies is lacking. Administration of charcoal, especially if mixed with sorbitol, can provoke vomiting, which could lead to pulmonary aspiration in an obtunded patient.
2. Contraindications—Activated charcoal should not be used for comatose or convulsing patients unless it can be given by gastric tube and the airway is first protected by a cuffed endotracheal tube. It is also contraindicated for patients with ileus or intestinal obstruction or those who have ingested corrosives for whom endoscopy is planned.
3. Technique—Administer activated charcoal, 60–100 g orally or via gastric tube, mixed in aqueous slurry. Repeated doses may be given to ensure gastrointestinal adsorption or to enhance elimination of some drugs.
B. Whole Bowel Irrigation
Whole bowel irrigation uses large volumes of a balanced polyethylene glycol-electrolyte solution to mechanically cleanse the entire intestinal tract. Because of the composition of the irrigating solution, there is no significant gain or loss of systemic fluids or electrolytes.
1. Indications—Whole bowel irrigation is particularly effective for massive iron ingestion in which intact tablets are visible on abdominal radiographs. It has also been used for ingestions of lithium, sustained-release and enteric-coated tablets, and swallowed drug-filled packets.
2. Contraindications—Do not use in patients with suspected intestinal obstruction. Use with caution in patients who are obtunded or have depressed airway protective reflexes.
3. Technique—Administer a balanced polyethylene glycol-electrolyte solution (CoLyte, GoLYTELY) into the stomach via gastric tube at a rate of 1–2 L/h until the rectal effluent is clear. This may take several hours. It is most effective when patients are able to sit on a commode to pass the intestinal contents.
C. Increased Drug Removal
1. Urinary manipulation—Forced diuresis is hazardous; the risk of complications (fluid overload, electrolyte imbalance) usually outweighs its benefits. Some drugs (eg, salicylates, phenobarbital) are more rapidly excreted with an alkaline urine. To alkalinize the urine, add 100 mEq (two ampules) of sodium bicarbonate to 1 L of 5% dextrose in 0.225% saline (¼ normal saline), and infuse this solution intravenously at a rate of about 150–200 mL/h. Acidification (sometimes promoted for amphetamines, phencyclidine) is not very effective and is contraindicated in the presence of rhabdomyolysis or myoglobinuria.
2. Hemodialysis—The indications for dialysis are as follows: (1) known or suspected potentially lethal amounts of a dialyzable drug (Table 38–4); (2) poisoning with deep coma, apnea, severe hypotension, fluid and electrolyte or acid-base disturbance, or extreme body temperature changes that cannot be corrected by conventional measures; or (3) poisoning in patients with severe kidney, cardiac, pulmonary, or hepatic disease who will not be able to eliminate toxin by the usual mechanisms.
Table 38–4. Recommended use of hemodialysis in poisoning.
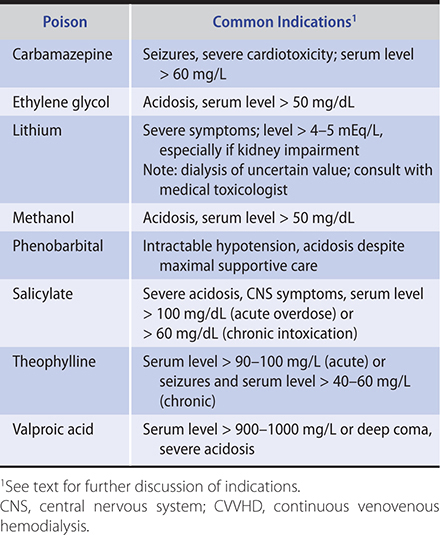
Continuous renal replacement therapy (including continuous venovenous hemodiafiltration and similar techniques) is of uncertain benefit for elimination of most poisons but has the advantage of gradual removal of the toxin and correction of any accompanying acidosis. Its use has been reported in the management of a variety of poisonings, including lithium intoxication.
3. Repeat-dose charcoal—Repeated doses of activated charcoal, 20–30 g orally or via gastric tube every 3–4 hours, may hasten elimination of some drugs (eg, phenytoin, carbamazepine, dapsone) by absorbing drugs excreted into the gut lumen (“gut dialysis”). However, clinical studies have failed to prove better outcome using repeat dose charcoal. Sorbitol or other cathartics should not be used with each dose, or else the resulting large stool volumes may lead to dehydration or hypernatremia.
Campion GH et al. Extracorporeal treatments in poisonings from four non-traditionally dialysed toxins (acetaminophen, digoxin, opioids and tricyclic antidepressants): a combined single-centre and national study. Basic Clin Pharmacol Toxicol. 2019 Mar;124(3):341–7. [PMID: 30248244]
Ghannoum M et al. Use of extracorporeal treatments in the management of poisonings. Kidney Int. 2018 Oct;94(4):682–8. [PMID: 29958694]
Zellner T et al. The use of activated charcoal to treat intoxications. Dtsch Arztebl Int. 2019 May 3;116(18):311–7. [PMID: 31219028]
DIAGNOSIS OF POISONING
The identity of the ingested substance or substances is usually known, but occasionally a comatose patient is found with an unlabeled container or the patient is unable or unwilling to give a coherent history. By performing a directed physical examination and ordering common clinical laboratory tests, the clinician can often make a tentative diagnosis that may allow empiric interventions or may suggest specific toxicologic tests.
 Physical Examination
Physical Examination
Important diagnostic variables in the physical examination include blood pressure, pulse rate, temperature, pupil size, sweating, muscle tone, level of consciousness, and the presence or absence of peristaltic activity. Poisonings may present with one or more of the following common syndromes.
A. Sympathomimetic Syndrome
The blood pressure and pulse rate are elevated, though with severe hypertension reflex bradycardia may occur. The temperature is often elevated, pupils are dilated, and the skin is sweaty, though mucous membranes are dry. Patients are usually agitated, anxious, or frankly psychotic.
Examples: Amphetamines, cocaine, ephedrine, pseudoephedrine, synthetic cathinones and cannabinoids.
B. Sympatholytic Syndrome
The blood pressure and pulse rate are decreased and body temperature is low. The pupils are small or even pinpoint. Patients are usually obtunded or comatose.
Examples: Barbiturates, benzodiazepines and other sedative hypnotics, gamma-hydroxybutyrate (GHB), clonidine and related antihypertensives, ethanol, opioids.
C. Cholinergic Syndrome
Stimulation of muscarinic receptors causes bradycardia, miosis (constricted pupils), sweating, and hyperperistalsis as well as bronchorrhea, wheezing, excessive salivation, and urinary incontinence. Nicotinic receptor stimulation may produce initial hypertension and tachycardia as well as fasciculations and muscle weakness. Patients are usually agitated and anxious.
Examples: Carbamates, nicotine, organophosphates (including nerve agents), physostigmine.
D. Anticholinergic Syndrome
Tachycardia with mild hypertension is common, and the body temperature is often elevated. Pupils are widely dilated. The skin is flushed, hot, and dry. Peristalsis is decreased, and urinary retention is common. Patients may have myoclonic jerking or choreoathetoid movements. Agitated delirium is frequently seen, and severe hyperthermia may occur.
Examples: Atropine, scopolamine, other naturally occurring and pharmaceutical anticholinergics, antihistamines, tricyclic antidepressants.
 Laboratory Tests
Laboratory Tests
The following clinical laboratory tests are recommended for screening of the overdosed patient: measured serum osmolality and calculated osmol gap, electrolytes and anion gap, glucose, creatinine, blood urea nitrogen (BUN), creatine kinase (CK), urinalysis (eg, oxalate crystals with ethylene glycol poisoning, myoglobinuria with rhabdomyolysis), and electrocardiography. Quantitative serum acetaminophen and ethanol levels should be determined in all patients with drug overdoses.
A. Osmol Gap
The osmol gap (Table 38–5) is increased in the presence of large quantities of low-molecular-weight substances, most commonly ethanol. Other common poisons associated with increased osmol gap are acetone, ethylene glycol, isopropyl alcohol, methanol, and propylene glycol. Note: Severe alcoholic ketoacidosis and diabetic ketoacidosis can also cause an elevated osmol gap resulting from the production of ketones and other low-molecular-weight substances.
Table 38–5. Use of the osmol gap in toxicology.
The osmol gap (Delta osm) is determined by subtracting the calculated serum osmolality from the measured serum osmolality.
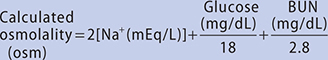
Delta osm = Measured osmolality – Calculated osmolality = 0 ± 10
Serum osmolality may be increased by contributions of exogenous substances such as alcohols and other low-molecular-weight substances. Since these substances are not included in the calculated osmolality, there will be a gap proportionate to their serum concentration. Contact a medical toxicologist or poison control center for assistance in calculating and interpreting the osmol gap.
Adapted, with permission, from Stone CK, Humphries RL (editors): Current Emergency Diagnosis & Treatment, 5th ed. McGraw-Hill, 2004.
B. Anion Gap
Metabolic acidosis associated with an elevated anion gap is usually due to an accumulation of lactic acid or other acids (see Chapter 21). Common causes of elevated anion gap in poisoning include carbon monoxide, cyanide, ethylene glycol, propylene glycol, medicinal iron, INH, methanol, metformin, ibuprofen, and salicylates. Massive acetaminophen overdose can cause early-onset anion gap metabolic acidosis.
The osmol gap should also be checked; combined elevated anion and osmol gaps suggests poisoning by methanol or ethylene glycol, though this may also occur in patients with diabetic ketoacidosis and alcoholic ketoacidosis.
C. Toxicology Laboratory Testing
A comprehensive toxicology screen is of little value in the initial care of the poisoned patient because results usually do not return in time to influence clinical management. Specific quantitative levels of certain drugs may be extremely helpful (Table 38–6), however, especially if specific antidotes or interventions (eg, dialysis) would be indicated based on the results.
Table 38–6. Specific quantitative levels and potential therapeutic interventions.1

Many hospitals can perform a quick but limited urine screen for “drugs of abuse” (typically these screens include only opiates, amphetamines, and cocaine, and some add benzodiazepines, barbiturates, methadone, oxycodone, phencyclidine, and tetrahydrocannabinol [marijuana]). There are numerous false-positive and false-negative results. For example, synthetic opioids, such as fentanyl, oxycodone, and methadone, are often not detected by routine opiate immunoassays.
 Abdominal Imaging
Abdominal Imaging
A plain film (or CT scan) of the abdomen may reveal radiopaque iron tablets, drug-filled condoms, or other toxic material. Studies suggest that few tablets are predictably visible (eg, ferrous sulfate, sodium chloride, calcium carbonate, and potassium chloride). Thus, the radiograph is useful only if abnormal.
 When to Refer
When to Refer
Consultation with a regional poison control center (1-800-222-1222) or a medical toxicologist is recommended when the diagnosis is uncertain; there are questions about what laboratory tests to order; when dialysis is being considered to remove the drug or poison; or when advice is needed regarding the indications, dose, and side effects of antidotes.
 When to Admit
When to Admit
• The patient has symptoms and signs of intoxication that are not expected to clear within a 6- to 8-hour observation period.
• Delayed absorption of the drug might be predicted to cause a later onset of serious symptoms (eg, after ingestion of a sustained-release product).
• Continued administration of an antidote is required (eg, N-acetylcysteine for acetaminophen overdose).
• Psychiatric or social services evaluation is needed for suicide attempt or suspected drug abuse.
Malek N et al. Common toxidromes in movement disorder neurology. Postgrad Med J. 2017 Jun;93(1100):326–32. [PMID: 28546460]
Nelson LS, Hoffman RS (editors). Goldfrank’s Toxicologic Emergencies, 11th ed. McGraw-Hill, 2019.
Olson KR (editor). Poisoning & Drug Overdose, 7th ed. McGraw-Hill, 2018.
Rasimas JJ et al. Assessment and management of toxidromes in the critical care unit. Crit Care Clin. 2017 Jul;33(3):521–41. [PMID: 28601133]
SELECTED POISONINGS
ACETAMINOPHEN
Acetaminophen (paracetamol in the United Kingdom, Europe) is a common analgesic found in many nonprescription and prescription products. After absorption, it is metabolized mainly by glucuronidation and sulfation, with a small fraction metabolized via the P450 mixed-function oxidase system (2E1) to a highly toxic reactive intermediate. This toxic intermediate is normally detoxified by cellular glutathione. With acute acetaminophen overdose (greater than 150–200 mg/kg, or 8–10 g in an average adult), hepatocellular glutathione is depleted and the reactive intermediate attacks other cell proteins, causing necrosis. Patients with enhanced P450 2E1 activity, such as those who chronically abuse alcohol and patients taking INH, are at increased risk for developing hepatotoxicity. Hepatic toxicity may also occur after overuse of acetaminophen—eg, as a result of taking two or three acetaminophen-containing products concurrently or exceeding the recommended maximum dose of 4 g/day for several days. The amount of acetaminophen in US oral prescription combination products (eg, hydrocodone/acetaminophen) is limited by the FDA to no more than 325 mg per tablet.
 Clinical Findings
Clinical Findings
Shortly after ingestion, patients may have nausea or vomiting, but there are usually no other signs of toxicity until 24–48 hours after ingestion, when hepatic aminotransferase levels begin to increase. With severe poisoning, fulminant hepatic necrosis may occur, resulting in jaundice, hepatic encephalopathy, acute kidney injury, and death. Rarely, massive ingestion (eg, serum levels greater than 500–1000 mg/L [33–66 mmol/L]) can cause early onset of acute coma, seizures, hypotension, and metabolic acidosis unrelated to hepatic injury.
The diagnosis after acute overdose is based on measurement of the serum acetaminophen level. Plot the serum level versus the time since ingestion on the acetaminophen nomogram shown in Figure 38–1. Ingestion of sustained-release products or coingestion of an anticholinergic agent, salicylate, or opioid drug may cause delayed elevation of serum levels, which can make it difficult to interpret the nomogram. The nomogram is also not useful after chronic or staggered overdose.
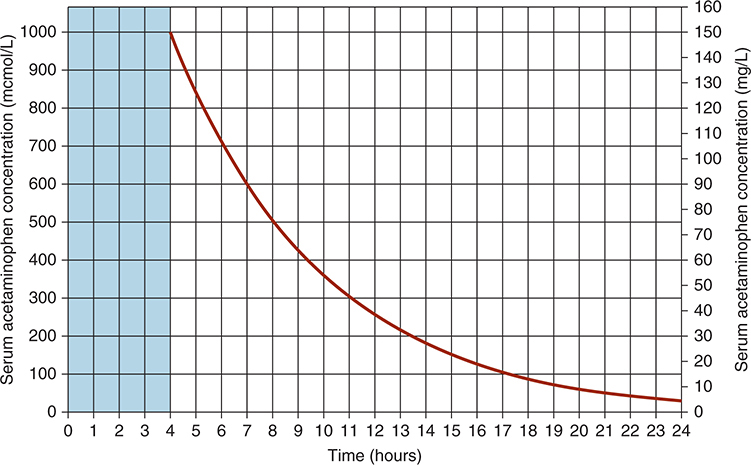
Figure 38–1. Nomogram for prediction of acetaminophen hepatotoxicity following acute overdosage. Patients with serum levels above the line after acute overdose should receive antidotal treatment. (Adapted, with permission, from Daly FF et al. Guidelines for the management of paracetamol poisoning in Australia and New Zealand—explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian Poisons Information Centres. Med J Austr. 2008;188:296. © Copyright 2008 The Medical Journal of Australia. By permission from John Wiley & Sons.)
 Treatment
Treatment
A. Emergency and Supportive Measures
Administer activated charcoal if it can be given within 1–2 hours of the ingestion. Although charcoal may interfere with absorption of the oral preparation of the antidote acetylcysteine, this is not considered clinically significant.
B. Specific Treatment
If the serum or plasma acetaminophen level falls above the line on the nomogram (Figure 38–1), treatment with N-acetylcysteine is indicated; it can be given orally or intravenously. Oral treatment begins with a loading dose of N-acetylcysteine, 140 mg/kg, followed by 70 mg/kg every 4 hours. Dilute the solution to about 5% with water, juice, or soda. If vomiting interferes with oral N-acetylcysteine administration, consider giving the antidote intravenously. The conventional oral N-acetylcysteine protocol in the United States calls for 72 hours of treatment. However, other regimens have demonstrated equivalent success with 20–48 hours of treatment.
The FDA-approved 21-hour intravenous regimen of acetylcysteine (Acetadote) calls for a loading dose of 150 mg/kg given intravenously over 60 minutes, followed by a 4-hour infusion of 50 mg/kg, and a 16-hour infusion of 100 mg/kg. (If Acetadote is not available, the conventional oral formulation may also be given intravenously using a micropore filter and a slow rate of infusion. Call a regional poison control center or medical toxicologist for assistance.)
Treatment with N-acetylcysteine is most effective if it is started within 8–10 hours after ingestion. Hemodialysis is rarely indicated, but might be needed in some patients with massive overdose.
Chiew AL et al. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst Rev. 2018 Feb 23;2:CD003328. [PMID: 29473717]
Lucyk S. Calculated decisions: acetaminophen overdose and N-acetylcysteine (NAC) dosing. Emerg Med Pract. 2018 Apr 1;20(4 Suppl):S3–5. [PMID: 29617550]
Wong A et al. Risk prediction of hepatotoxicity in paracetamol poisoning. Clin Toxicol (Phila). 2017 Sep;55(8):879–92. [PMID: 28447858]
Woodhead K et al. BET 1: In paracetamol overdose, is oral N-acetylcysteine as effective as intravenous N-acetylcysteine? Emerg Med J. 2018 Oct;35(10):643–5. [PMID: 30249712]
ACIDS, CORROSIVE
The strong mineral acids exert primarily a local corrosive effect on the skin and mucous membranes. Symptoms include severe pain in the throat and upper gastrointestinal tract; bloody vomitus; difficulty in swallowing, breathing, and speaking; discoloration and destruction of skin and mucous membranes in and around the mouth; and shock. Severe systemic metabolic acidosis may occur both as a result of cellular injury and from systemic absorption of the acid.
Severe deep destructive tissue damage may occur after exposure to hydrofluoric acid because of the penetrating and highly toxic fluoride ion. Systemic hypocalcemia and hyperkalemia may also occur after fluoride absorption, even following skin exposure.
Inhalation of volatile acids, fumes, or gases such as chlorine, fluorine, bromine, or iodine causes severe irritation of the throat and larynx and may cause upper airway obstruction and noncardiogenic pulmonary edema.
 Treatment
Treatment
A. Ingestion
Dilute immediately by giving a glass (4–8 oz) of water to drink. Do not give bicarbonate or other neutralizing agents, and do not induce vomiting. Some experts recommend immediate cautious placement of a small flexible gastric tube and removal of stomach contents followed by lavage, particularly if the corrosive is a liquid or has important systemic toxicity.
In symptomatic patients, perform flexible endoscopic esophagoscopy to determine the presence and extent of injury. CT scan or plain radiographs of the chest and abdomen may also reveal the extent of injury. Perforation, peritonitis, and major bleeding are indications for surgery.
B. Skin Contact
Flood with water for 15 minutes. Use no chemical antidotes; the heat of the reaction may cause additional injury.
For hydrofluoric acid burns, soak the affected area in benzalkonium chloride solution or apply 2.5% calcium gluconate gel (prepared by adding 3.5 g calcium gluconate to 5 oz of water-soluble surgical lubricant, eg, K-Y Jelly); then arrange immediate consultation with a plastic surgeon or other specialist. Binding of the fluoride ion may be achieved by injecting 0.5 mL of 5% calcium gluconate per square centimeter under the burned area. (Caution: Do not use calcium chloride.) Use of a Bier-block technique or intra-arterial infusion of calcium is sometimes required for extensive burns or those involving the nail bed; consult with a hand surgeon or poison control center (1-800-222-1222).
C. Eye Contact
Anesthetize the conjunctiva and corneal surfaces with topical local anesthetic drops (eg, proparacaine). Flood with water for 15 minutes, holding the eyelids open. Check pH with pH 6.0–8.0 test paper, and repeat irrigation, using 0.9% saline, until pH is near 7.0. Check for corneal damage with fluorescein and slit-lamp examination; consult an ophthalmologist about further treatment.
D. Inhalation
Remove from further exposure to fumes or gas. Check skin and clothing. Observe for and treat chemical pneumonitis or pulmonary edema.
Bird JH et al. Controversies in the management of caustic ingestion injury: an evidence-based review. Clin Otolaryngol. 2017 Jun;42(3):701–8. [PMID: 28032947]
Cowan T et al. Acute esophageal injury and strictures following corrosive ingestions in a 27-year cohort. Am J Emerg Med. 2017 Mar;35(3):488–92. [PMID: 27955797]
Han HH et al. Importance of initial management and surgical treatment after hydrofluoric acid burn of the finger. Burns. 2017 Feb;43(1):e1–6. [PMID: 27650188]
Methasate A et al. Role of endoscopy in caustic injury of the esophagus. World J Gastrointest Endosc. 2018 Oct 16;10(10):274–82. [PMID: 30364838]
Pu Q et al. Extracorporeal membrane oxygenation combined with continuous renal replacement therapy in cutaneous burn and inhalation injury caused by hydrofluoric acid and nitric acid. Medicine (Baltimore). 2017 Dec;96(48):e8972. [PMID: 29310404]
ALKALIES
The strong alkalies are common ingredients of some household cleaning compounds and may be suspected by their “soapy” texture. Those with alkalinity above pH 12.0 are particularly corrosive. Disk (or “button”) batteries are also a source. Alkalies cause liquefactive necrosis, which is deeply penetrating. Symptoms include burning pain in the upper gastrointestinal tract, nausea, vomiting, and difficulty in swallowing and breathing. Examination reveals destruction and edema of the affected skin and mucous membranes and bloody vomitus and stools. Radiographs may reveal evidence of perforation or the presence of radiopaque disk batteries in the esophagus or lower gastrointestinal tract.
 Treatment
Treatment
A. Ingestion
Dilute immediately with a glass of water. Do not induce emesis. Some gastroenterologists recommend immediate cautious placement of a small flexible gastric tube and removal of stomach contents followed by gastric lavage after ingestion of liquid caustic substances, in order to remove residual material. However, others argue that passage of a gastric tube is contraindicated due to the risk of perforation or reexposure of the esophagus to the corrosive material from vomiting around the tube.
Prompt endoscopy is recommended in symptomatic patients to evaluate the extent of damage; CT scanning may also aid in assessment. If a radiograph reveals ingested disk batteries lodged in the esophagus, immediate endoscopic removal is mandatory.
The use of corticosteroids to prevent stricture formation is of no proved benefit and is definitely contraindicated if there is evidence of esophageal perforation.
B. Skin Contact
Wash with running water until the skin no longer feels soapy. Relieve pain and treat shock.
C. Eye Contact
Anesthetize the conjunctival and corneal surfaces with topical anesthetic (eg, proparacaine). Irrigate with water or saline continuously for 20–30 minutes, holding the lids open. Amphoteric solutions may be more effective than water or saline and some are available in Europe (Diphoterine, Prevor). Check pH with pH test paper and repeat irrigation for additional 30-minute periods until the pH is near 7.0. Check for corneal damage with fluorescein and slit-lamp examination; consult an ophthalmologist for further treatment.
Bizrah M et al. An update on chemical eye burns. Eye (Lond). 2019 Sep;33(9):1362–77. [PMID: 31086244]
Dohlman CH et al. Chemical burns of the eye: the role of retinal injury and new therapeutic possibilities. Cornea. 2018 Feb;37(2):248–51. [PMID: 29135604]
Zhang X et al. Tractional Descemet’s membrane detachment after ocular alkali burns: case reports and review of literature. BMC Ophthalmol. 2018 Sep 24;18(1):256. [PMID: 30249214]
AMPHETAMINES & COCAINE
Amphetamines and cocaine are widely abused for their euphorigenic and stimulant properties. Both drugs may be smoked, snorted, ingested, or injected. Amphetamines and cocaine produce central nervous system stimulation and a generalized increase in central and peripheral sympathetic activity. The toxic dose of each drug is highly variable and depends on the route of administration and individual tolerance. The onset of effects is most rapid after intravenous injection or smoking. Amphetamine derivatives and related drugs include methamphetamine (“crystal meth,” “crank”), MDMA (“Ecstasy”), ephedrine (“herbal ecstasy”), and methcathinone (“cat” or “khat”). Methcathinone derivatives and related synthetic chemicals such as methylenedioxypyrovalerone (MDPV) have become popular drugs of abuse and are often sold as purported “bath salts.” Amphetamine-like reactions have also been reported after use of synthetic cannabinoids (eg, “Spice” and “K2”). Nonprescription medications and nutritional supplements may contain stimulant or sympathomimetic drugs such as ephedrine, yohimbine, or caffeine (see also Theophylline & Caffeine section).
 Clinical Findings
Clinical Findings
Presenting symptoms may include anxiety, tremulousness, tachycardia, hypertension, diaphoresis, dilated pupils, agitation, muscular hyperactivity, and psychosis. Muscle hyperactivity may lead to metabolic acidosis and rhabdomyolysis. In severe intoxication, seizures and hyperthermia may occur. Sustained or severe hypertension may result in intracranial hemorrhage, aortic dissection, or myocardial infarction; chronic use may cause cardiomyopathy. Ischemic colitis has been reported. Hyponatremia has been reported after MDMA use; the mechanism is not known but may involve excessive water intake, syndrome of inappropriate antidiuretic hormone (SIADH), or both.
The diagnosis is supported by finding amphetamines or the cocaine metabolite benzoylecgonine in the urine. Note that many drugs can give false-positive results on the immunoassay for amphetamines, and most synthetic stimulants do not react with the immunoassay, giving false-negative results.
 Treatment
Treatment
A. Emergency and Supportive Measures
Maintain a patent airway and assist ventilation, if necessary. Treat seizures as described at the beginning of this chapter. Rapidly lower the body temperature in patients who are hyperthermic (temperature higher than 39–40°C). Give intravenous fluids to prevent myoglobinuric kidney injury in patients who have rhabdomyolysis.
B. Specific Treatment
Treat agitation, psychosis, or seizures with a benzodiazepine such as diazepam, 5–10 mg, or lorazepam, 2–3 mg intravenously. Add phenobarbital 15 mg/kg intravenously for persistent seizures. Treat hypertension with a vasodilator drug such as phentolamine (1–5 mg intravenously) or nitroprusside, or a combined alpha- and beta-adrenergic blocker such as labetalol (10–20 mg intravenously). Do not administer a pure beta-blocker such as propranolol alone, as this may result in paradoxic worsening of the hypertension as a result of unopposed alpha-adrenergic effects.
Treat tachycardia or tachyarrhythmias with a short-acting beta-blocker such as esmolol (25–100 mcg/kg/min by intravenous infusion). Treat hyperthermia as described above. Treat hyponatremia as outlined in Chapter 21.
Rahimi M et al. Predictive factors of mortality in acute amphetamine type stimulants poisoning; a review of 226 cases. Emerg (Tehran). 2018;6(1):e1. [PMID: 29503826]
Richards JR et al. Methamphetamine use and heart failure: prevalence, risk factors, and predictors. Am J Emerg Med. 2018 Aug;36(8):1423–8. [PMID: 29307766]
Stockings E et al. Mortality among people with regular or problematic use of amphetamines: a systematic review and meta-analysis. Addiction. 2019 Oct;114(10):1738–50. [PMID: 31180607]
White CM. The pharmacologic and clinical effects of illicit synthetic cannabinoids. J Clin Pharmacol. 2017 Mar;57(3):297–304. [PMID: 27610597]
Williams MV. Cannabinoids: emerging evidence in use and abuse. Emerg Med Pract. 2018 Aug;20(8):1–20. [PMID: 30020736]
ANTICOAGULANTS
Warfarin and related compounds (including ingredients of many commercial rodenticides, the so-called superwarfarins such as brodifacoum, difenacoum, and related compounds) inhibit the normal clotting system by blocking hepatic synthesis of vitamin K–dependent clotting factors. After ingestion of “superwarfarins,” inhibition of clotting factor synthesis may persist for several weeks or even months after a single dose. Newer oral anticoagulants include the direct thrombin inhibitor dabigatran and the factor Xa inhibitors apixiban, betrixaban, edoxaban, and rivaroxaban. Some of these, especially dabigatran, are largely eliminated by the kidney and may accumulate in patients with kidney dysfunction.
Excessive anticoagulation may cause hemoptysis, gross hematuria, bloody stools, hemorrhages into organs, widespread bruising, and bleeding into joint spaces.
 Treatment
Treatment
A. Emergency and Supportive Measures
Discontinue the drug at the first sign of gross bleeding, and determine the prothrombin time (international normalized ratio, INR). The prothrombin time is increased within 12–24 hours (peak 36–48 hours) after overdose of warfarin or “superwarfarins.” Note: The newer oral anticoagulants (dabigatran, apixiban, betrixaban, edoxaban, and rivaroxaban) do not predictably alter the prothrombin time; however, a normal INR suggests no significant toxicity.
If the patient has ingested an acute overdose, administer activated charcoal.
B. Specific Treatment
1. Warfarin—In cases of warfarin and “superwarfarin” overdose, do not treat prophylactically with vitamin K—wait for evidence of anticoagulation (elevated prothrombin time). See Table 14–21 for the management of INR above therapeutic range. Doses of vitamin K as high as 200 mg/day have been required after ingestion of “superwarfarins.” Give fresh-frozen plasma, prothrombin complex concentrate, or activated factor VII as needed to rapidly correct the coagulation factor deficit if there is serious bleeding. If the patient is chronically anticoagulated and has strong medical indications for being maintained in that status (eg, prosthetic heart valve), give much smaller doses of vitamin K (1 mg orally) and fresh-frozen plasma (or both) to titrate to the desired prothrombin time. If the patient has ingested brodifacoum or a related superwarfarin, prolonged observation (over weeks) and repeated administration of large doses of vitamin K may be required.
2. Direct-acting oral anticoagulants—Vitamin K does not reverse the anticoagulant effects of the direct-acting oral anticoagulants. Idarucizumab has been approved by the FDA for reversal of the thrombin inhibitor dabigatran; andexanet is approved for reversal of the factor Xa inhibitors apixaban, edoxaban, betrixaban, and rivaroxaban. The efficacy of fresh-frozen plasma and clotting factor concentrates is uncertain.
Berling I et al. Warfarin poisoning with delayed rebound toxicity. J Emerg Med. 2017 Feb;52(2):194–6. [PMID: 27838137]
Cuker A et al. Reversal of direct oral anticoagulants: guidance from the Anticoagulation Forum. Am J Hematol. 2019 Jun;94(6):697–709. [PMID: 30916798]
Dobesh PP et al. Antidotes for reversal of direct oral anticoagulants. Pharmacol Ther. 2019 Dec;204:107405. [PMID: 31521696]
Levine M et al. Assessing bleeding risk in patients with intentional overdoses of novel antiplatelet and anticoagulant medications. Ann Emerg Med. 2018 Mar;71(3):273–8. [PMID: 29032872]
ANTICONVULSANTS
Anticonvulsants (carbamazepine, phenytoin, valproic acid, and many newer agents) are widely used in the management of seizure disorders and some are also used for treatment of mood disorders or pain.
Phenytoin can be given orally or intravenously. Rapid intravenous injection of phenytoin can cause acute myocardial depression and cardiac arrest owing to the solvent propylene glycol (fosphenytoin does not contain this diluent). Chronic phenytoin intoxication can occur following only slightly increased doses because of zero-order kinetics and a small toxic-therapeutic window. Phenytoin intoxication can also occur following acute intentional or accidental overdose. The overdose syndrome is usually mild even with high serum levels. The most common manifestations are ataxia, nystagmus, and drowsiness. Choreoathetoid movements have been described.
Carbamazepine intoxication causes drowsiness, stupor and, with high levels, atrioventricular block, coma, and seizures. Dilated pupils and tachycardia are common. Toxicity may be seen with serum levels over 20 mg/L (85 mcmol/L), although severe poisoning is usually associated with concentrations greater than 30–40 mg/L (127–169 mcmol/L). Because of erratic and slow absorption, intoxication may progress over several hours to days.
Valproic acid intoxication produces a unique syndrome consisting of hypernatremia (from the sodium component of the salt), metabolic acidosis, hypocalcemia, elevated serum ammonia, and mild liver aminotransferase elevation. Hypoglycemia may occur as a result of hepatic metabolic dysfunction. Coma with small pupils may be seen and can mimic opioid poisoning. Encephalopathy and cerebral edema can occur.
Gabapentin, levetiracetam, vigabatrin, and zonisamide generally cause somnolence, confusion, and dizziness; there is one case report of hypotension and bradycardia after a large overdose of levetiracetam. Felbamate can cause crystalluria and kidney injury after overdose and may cause idiosyncratic aplastic anemia with therapeutic use. Lamotrigine, topiramate, and tiagabine have been reported to cause seizures after overdose; lamotrigine has sodium channel–blocking properties and may cause QRS prolongation and heart block.
 Treatment
Treatment
A. Emergency and Supportive Measures
For recent ingestions, give activated charcoal orally or by gastric tube. For large ingestions of carbamazepine or valproic acid—especially of sustained-release formulations—consider whole bowel irrigation.
B. Specific Treatment
There are no specific antidotes. Naloxone was reported to have reversed valproic acid overdose in one anecdotal case. Carnitine (and possibly l-arginine) may be useful in patients with valproic acid–induced hyperammonemia. Consider hemodialysis for massive intoxication with valproic acid or carbamazepine (eg, carbamazepine levels greater than 60 mg/L [254 mcmol/L] or valproic acid levels greater than 800 mg/L [5544 mcmol/L]).
Alyahya B et al. Acute lamotrigine overdose: a systematic review of published adult and pediatric cases. Clin Toxicol (Phila). 2018 Feb;56(2):81–9. [PMID: 28862044]
Kalogera V et al. Patient survival after acute voluntary poisoning with a huge dose of oxcarbazepine and olanzapine. Med Arch. 2018 Oct;72(4):303–5. [PMID: 30515002]
Mahmoud SH. Antiepileptic drug removal by continuous renal replacement therapy: a review of the literature. Clin Drug Investig. 2017 Jan;37(1):7–23. [PMID: 27587068]
Yang X et al. Early hemoperfusion for emergency treatment of carbamazepine poisoning. Am J Emerg Med. 2018 Jun;36(6):926–30. [PMID: 29066188]
ANTIPSYCHOTIC DRUGS
Drugs in this group include “conventional” antipsychotics (eg, chlorpromazine, haloperidol, droperidol) and newer “atypical” antipsychotics (eg, risperidone, olanzapine, ziprasidone, quetiapine, aripiprazole). While conventional drugs act mainly on CNS dopamine receptors, atypical drugs also interact with serotonin receptors.
Therapeutic doses of conventional phenothiazines (particularly chlorpromazine) induce drowsiness and mild orthostatic hypotension in as many as 50% of patients. Larger doses can cause obtundation, miosis, severe hypotension, tachycardia, convulsions, and coma. Abnormal cardiac conduction may occur, resulting in prolongation of QRS or QT intervals (or both) and ventricular arrhythmias. Among the atypical agents, quetiapine is more likely to cause coma and hypotension. Hypotension is probably related to blockade of peripheral alpha-adrenergic receptors, causing vasodilatation.
With therapeutic or toxic doses, an acute extrapyramidal dystonic reaction may develop in some patients, with spasmodic contractions of the face and neck muscles, extensor rigidity of the back muscles, carpopedal spasm, and motor restlessness. This reaction is more common with haloperidol and other butyrophenones and less common with newer atypical antipsychotics. Severe rigidity accompanied by hyperthermia and metabolic acidosis (“neuroleptic malignant syndrome”) may occasionally occur and is life-threatening (see Chapter 25). Atypical antipsychotics have also been associated with weight gain and diabetes mellitus, including diabetic ketoacidosis.
 Treatment
Treatment
A. Emergency and Supportive Measures
Administer activated charcoal for large or recent ingestions. For severe hypotension, treatment with intravenous fluids and vasopressor agents may be necessary. Treat hyperthermia as outlined. Maintain ECG monitoring.
B. Specific Treatment
Hypotension often responds to intravenous saline boluses; cardiac arrhythmias associated with widened QRS intervals on the ECG may respond to intravenous sodium bicarbonate as is given for tricyclic antidepressant overdoses. Prolongation of the QT interval and torsades de pointes is usually treated with intravenous magnesium or overdrive pacing.
For extrapyramidal signs, give diphenhydramine, 0.5–1 mg/kg intravenously, or benztropine mesylate, 0.01–0.02 mg/kg intramuscularly. Treatment with oral doses of these agents should be continued for 24–48 hours.
Bromocriptine (2.5–7.5 mg orally daily) may be effective for mild or moderate neuroleptic malignant syndrome. Dantrolene (2–5 mg/kg intravenously) has also been used for muscle rigidity but is not a true antidote. For severe hyperthermia, rapid neuromuscular paralysis is preferred.
Beach SR et al. QT prolongation, torsades de pointes, and psychotropic medications: a 5-year update. Psychosomatics. 2018 Mar–Apr;59(2):105–22. [PMID: 29275963]
Christensen AP et al. Overdoses with aripiprazole: signs, symptoms and outcome in 239 exposures reported to the Danish Poison Information Centre. Basic Clin Pharmacol Toxicol. 2018 Feb;122(2):293–8. [PMID: 28881461]
Peridy E et al. Quetiapine poisoning and factors influencing severity. J Clin Psychopharmacol. 2019 Jul/Aug;39(4):312–7. [PMID: 31205192]
ARSENIC
Arsenic is found in some pesticides and industrial chemicals and is used as a chemotherapeutic agent. Chronic arsenic poisoning has been associated with contaminated aquifers used for drinking water. Symptoms of acute poisoning usually appear within 1 hour after ingestion but may be delayed as long as 12 hours. They include abdominal pain, vomiting, watery diarrhea, and skeletal muscle cramps. Profound dehydration and shock may occur. In chronic poisoning, symptoms can be vague but often include pancytopenia, painful peripheral sensory neuropathy, and skin changes including melanosis, keratosis, and desquamating rash. Cancers of the lung, bladder, and skin have been reported. Urinary arsenic levels may be falsely elevated after certain meals (eg, seafood) that contain large quantities of a nontoxic form of organic arsenic.
 Treatment
Treatment
A. Emergency Measures
After recent ingestion (within 1–2 hours), perform gastric lavage. Activated charcoal is of uncertain benefit because it binds arsenic poorly. Administer intravenous fluids to replace losses due to vomiting and diarrhea.
B. Antidote
For patients with severe acute intoxication, administer a chelating agent. The preferred drug is 2,3-dimercaptopropanesulfonic acid (DMPS, Unithiol) (3–5 mg/kg intravenously every 4 hours); although there is no FDA-approved commercial formulation of DMPS in the United States, it can be obtained from some compounding pharmacies. An alternative parenteral chelator is dimercaprol (British anti-Lewisite, BAL), which comes as a 10% solution in peanut oil, and is given 3–5 mg/kg intramuscularly every 4–6 hours for 2 days. The side effects include nausea, vomiting, headache, and hypertension. When gastrointestinal symptoms allow, switch to the oral chelator succimer (dimercaptosuccinic acid, DMSA), 10 mg/kg every 8 hours, for 1 week. Consult a medical toxicologist or regional poison control center (1-800-222-1222) for advice regarding chelation.
Arslan B et al. Arsenic: a review on exposure pathways, accumulation, mobility and transmission into the human food chain. Rev Environ Contam Toxicol. 2017;243:27–51. [PMID: 28005215]
Dani SU et al. Chronic arsenic intoxication diagnostic score (CAsIDS). J Appl Toxicol. 2018 Jan;38(1):122–44. [PMID: 28857213]
Lu PH et al. Survival without peripheral neuropathy after massive acute arsenic poisoning: treated by 2,3-dimercaptopropane-1-sulphonate. J Clin Pharm Ther. 2017 Aug;42(4):506–8. [PMID: 28547870]
ATROPINE & ANTICHOLINERGICS
Atropine, scopolamine, belladonna, Datura stramonium, Hyoscyamus niger, some mushrooms, tricyclic antidepressants, and antihistamines are antimuscarinic agents with variable central nervous system effects. Symptoms of toxicity include dryness of the mouth, thirst, difficulty in swallowing, and blurring of vision. Physical signs include dilated pupils, flushed skin, tachycardia, fever, delirium, myoclonus, and ileus. Antidepressants and antihistamines may also induce convulsions.
Antihistamines are commonly available with or without prescription. Diphenhydramine commonly causes delirium, tachycardia, and seizures. Massive diphenhydramine overdose may mimic tricyclic antidepressant cardiotoxic poisoning.
 Treatment
Treatment
A. Emergency and Supportive Measures
Administer activated charcoal. External cooling and sedation, or neuromuscular paralysis in rare cases, are indicated to control high temperatures.
B. Specific Treatment
For severe anticholinergic syndrome (eg, agitated delirium), give physostigmine salicylate, 0.5–1 mg slowly intravenously over 5 minutes, with ECG monitoring; repeat as needed to a total dose of no more than 2 mg. Caution: Bradyarrhythmias and convulsions are a hazard with physostigmine administration, and the drug should be avoided in patients with evidence of cardiotoxic effects (eg, QRS interval prolongation) from tricyclic antidepressants or other sodium channel blockers.
Chung WM et al. Datura fruit poisoning. Med J Malaysia. 2018 Dec;73(6):453–4. [PMID: 30647232]
Jayawickreme KP et al. Unknowing ingestion of Brugmansia suaveolens leaves presenting with signs of anticholinergic toxicity: a case report. J Med Case Rep. 2019 Oct 30;13(1):322. [PMID: 31665073]
Zhang XC et al. Postoperative anticholinergic poisoning: concealed complications of a commonly used medication. J Emerg Med. 2017 Oct;53(4):520–3. [PMID: 28756934]
BETA-ADRENERGIC BLOCKERS
There are a wide variety of beta-adrenergic blocking drugs, with varying pharmacologic and pharmacokinetic properties (see Table 11–9). The most toxic beta-blocker is propranolol, which not only blocks beta-1 and beta-2 adrenoceptors but also has direct membrane-depressant and central nervous system effects.
 Clinical Findings
Clinical Findings
The most common findings with mild or moderate intoxication are hypotension and bradycardia. Cardiac depression from more severe poisoning is often unresponsive to conventional therapy with beta-adrenergic stimulants such as dopamine and norepinephrine. In addition, with propranolol and other lipid-soluble drugs, seizures and coma may occur. Propranolol, oxprenolol, acebutolol, and alprenolol also have membrane-depressant effects and can cause conduction disturbance (wide QRS interval) similar to tricyclic antidepressant overdose.
The diagnosis is based on typical clinical findings. Routine toxicology screening does not usually include beta-blockers.
 Treatment
Treatment
A. Emergency and Supportive Measures
Attempts to treat bradycardia or heart block with atropine (0.5–2 mg intravenously), isoproterenol (2–20 mcg/min by intravenous infusion, titrated to the desired heart rate), or an external transcutaneous cardiac pacemaker are often ineffective, and specific antidotal treatment may be necessary.
For drugs ingested within an hour of presentation (or longer after ingestion of an extended-release formulation), administer activated charcoal.
B. Specific Treatment
For persistent bradycardia and hypotension, give glucagon, 5–10 mg intravenously, followed by an infusion of 1–5 mg/h. Glucagon is an inotropic agent that acts at a different receptor site and is therefore not affected by beta-blockade. High-dose insulin (0.5–1 unit/kg/h intravenously) along with glucose supplementation has also been used to reverse severe cardiotoxicity. Membrane-depressant effects (wide QRS interval) may respond to boluses of sodium bicarbonate (50–100 mEq intravenously) as for tricyclic antidepressant poisoning. Intravenous lipid emulsion (Intralipid 20%, 1.5 mL/kg) has been used successfully in severe propranolol overdose.
Krenz JR et al. An overview of hyperinsulinemic-euglycemic therapy in calcium channel blocker and β-blocker overdose. Pharmacotherapy. 2018 Nov;38(11):1130–42. [PMID: 30141827]
Seegobin K et al. Severe beta blocker and calcium channel blocker overdose: role of high dose insulin. Am J Emerg Med. 2018 Apr;36(4):736.e5–6. [PMID: 29331270]
CALCIUM CHANNEL BLOCKERS
In therapeutic doses, nifedipine, nicardipine, amlodipine, felodipine, isradipine, nisoldipine, and nimodipine act mainly on blood vessels, while verapamil and diltiazem act mainly on cardiac contractility and conduction. However, these selective effects can be lost after acute overdose. Patients may present with bradycardia, atrioventricular (AV) nodal block, hypotension, or a combination of these effects. Hyperglycemia is common due to blockade of insulin release. With severe poisoning, cardiac arrest may occur.
 Treatment
Treatment
A. Emergency and Supportive Measures
For ingested drugs, administer activated charcoal. In addition, whole bowel irrigation should be initiated as soon as possible if the patient has ingested a sustained-release product.
B. Specific Treatment
Treat symptomatic bradycardia with atropine (0.5–2 mg intravenously), isoproterenol (2–20 mcg/min by intravenous infusion), or a transcutaneous cardiac pacemaker. For hypotension, give calcium chloride 10%, 10 mL, or calcium gluconate 10%, 20 mL. Repeat the dose every 3–5 minutes. The optimum (or maximum) dose has not been established, but many toxicologists recommend raising the ionized serum calcium level to as much as twice the normal level. Calcium is most useful in reversing negative inotropic effects and is less effective for AV nodal blockade and bradycardia. High doses of insulin (0.5–1 unit/kg intravenous bolus followed by 0.5–1 unit/kg/h infusion) along with sufficient dextrose to maintain euglycemia have been reported to be beneficial, but there are no controlled studies. Infusion of Intralipid 20% lipid emulsion has been reported to improve hemodynamics in animal models and case reports of calcium channel blocker poisoning. Methylene blue (1–2 mg/kg) was reported to reverse refractory shock due to profound vasodilation in a patient with amlodipine poisoning. ECMO has been recommended for refractory shock.
Christensen MB et al. Outcomes following calcium channel blocker exposures reported to a poison information center. BMC Pharmacol Toxicol. 2018 Nov 27;19(1):78. [PMID: 30482251]
Maskell KF et al. Survival after cardiac arrest: ECMO rescue therapy after amlodipine and metoprolol overdose. Cardiovasc Toxicol. 2017 Apr;17(2):223–5. [PMID: 26913719]
Ramanathan K et al. Extracorporeal therapy for amlodipine poisoning. J Artif Organs. 2020 Jun;23(2):183–6. [PMID: 31552515]
St-Onge M et al. Experts consensus recommendations for the management of calcium channel blocker poisoning in adults. Crit Care Med. 2017 Mar;45(3):e306–15. [PMID: 27749343]
CARBON MONOXIDE
Carbon monoxide is a colorless, odorless gas produced by the combustion of carbon-containing materials. Poisoning may occur as a result of suicidal or accidental exposure to automobile exhaust, smoke inhalation in a fire, or accidental exposure to an improperly vented gas heater, generator, or other appliance. Carbon monoxide can be generated during degradation of some anesthetic gases by carbon dioxide adsorbents. Carbon monoxide avidly binds to hemoglobin, with an affinity approximately 250 times that of oxygen. This results in reduced oxygen-carrying capacity and altered delivery of oxygen to cells (see also Smoke Inhalation in Chapter 9).
 Clinical Findings
Clinical Findings
At low carbon monoxide levels (carboxyhemoglobin saturation 10–20%), victims may have headache, dizziness, abdominal pain, and nausea. With higher levels, confusion, dyspnea, and syncope may occur. Hypotension, coma, and seizures are common with levels greater than 50–60%. Survivors of acute severe poisoning may develop permanent obvious or subtle neurologic and neuropsychiatric deficits. The fetus and newborn may be more susceptible because of high carbon monoxide affinity for fetal hemoglobin.
Carbon monoxide poisoning should be suspected in any person with severe headache or acutely altered mental status, especially during cold weather, when improperly vented heating systems may have been used. Diagnosis depends on specific measurement of the arterial or venous carboxyhemoglobin saturation, although the level may have declined if high-flow oxygen therapy has already been administered, and levels do not always correlate with clinical symptoms. Routine arterial blood gas testing and pulse oximetry are not useful because they give falsely normal PaO2 and oxyhemoglobin saturation determinations, respectively. (A specialized pulse oximetry device, the Masimo pulse CO-oximeter, is capable of distinguishing oxyhemoglobin from carboxyhemoglobin.)
 Treatment
Treatment
A. Emergency and Supportive Measures
Maintain a patent airway and assist ventilation, if necessary. Remove the victim from exposure. Treat patients with coma, hypotension, or seizures as described at the beginning of this chapter.
B. Specific Treatment
The half-life of the carboxyhemoglobin (CoHb) complex is about 4–5 hours in room air but is reduced dramatically by high concentrations of oxygen. Administer 100% oxygen by tight-fitting high-flow reservoir face mask or endotracheal tube. Hyperbaric oxygen (HBO) can provide 100% oxygen under higher than atmospheric pressures, further shortening the half-life; it may also reduce the incidence of subtle neuropsychiatric sequelae. Randomized controlled studies disagree about the benefit of HBO, but commonly recommended indications for HBO in patients with carbon monoxide poisoning include a history of loss of consciousness, CoHb greater than 25%, metabolic acidosis, age over 50 years, and cerebellar findings on neurologic examination.
Eichhorn L et al. The diagnosis and treatment of carbon monoxide poisoning. Dtsch Arztebl Int. 2018 Dec 24;115(51–52):863–70. [PMID: 30765023]
Lin CH et al. Treatment with normobaric or hyperbaric oxygen and its effect on neuropsychometric dysfunction after carbon monoxide poisoning: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018 Sep;97(39):e12456. [PMID: 30278526]
Rose JJ et al. Carbon monoxide poisoning: pathogenesis, management, and future directions of therapy. Am J Respir Crit Care Med. 2017 Mar 1;195(5):596–606. Erratum in: Am J Respir Crit Care Med. 2017 Aug 1;196(3):398–9. [PMID: 27753502]
CHEMICAL WARFARE: NERVE AGENTS
Nerve agents used in chemical warfare work by cholinesterase inhibition and are most commonly organophosphorus compounds. Agents such as tabun (GA), sarin (GB), soman (GD), and VX are similar to insecticides such as malathion but are vastly more potent. They may be inhaled or absorbed through the skin. Systemic effects due to unopposed action of acetylcholine include miosis, salivation, abdominal cramps, diarrhea, and muscle paralysis producing respiratory arrest. Inhalation also produces severe bronchoconstriction and copious nasal and tracheobronchial secretions.
 Treatment
Treatment
A. Emergency and Supportive Measures
Perform thorough decontamination of exposed areas with repeated soap and shampoo washing. Personnel caring for such patients must wear protective clothing and gloves, since cutaneous absorption may occur through normal skin.
B. Specific Treatment
Give atropine in an initial dose of 2 mg intravenously and repeat as needed to reverse signs of acetylcholine excess. (Some victims have required several hundred milligrams.) Treat also with the cholinesterase-reactivating agent pralidoxime, 1–2 g intravenously initially followed by an infusion at a rate of 200–400 mg/h.
Agency for Toxic Substances and Disease Registry. Toxic Substances Portal. June 20, 2018. https://www.atsdr.cdc.gov/substances/index.asp
Candiotti K. A primer on nerve agents: what the emergency responder, anesthesiologist, and intensivist needs to know. Can J Anaesth. 2017 Oct;64(10):1059–70. [PMID: 28766156]
Hulse EJ et al. Organophosphorus nerve agent poisoning: managing the poisoned patient. Br J Anaesth. 2019 Oct;123(4):457–63. [PMID: 31248646]
Richardson JR et al. Neurotoxicity of pesticides. Acta Neuropathol. 2019 Sep;138(3):343–62. [PMID: 31197504]
Timperley CM et al. Advice on assistance and protection from the Scientific Advisory Board of the Organisation for the Prohibition of Chemical Weapons: Part 2. On preventing and treating health effects from acute, prolonged, and repeated nerve agent exposure, and the identification of medical countermeasures able to reduce or eliminate the longer-term health effects of nerve agents. Toxicology. 2019 Feb 1;413:13–23. [PMID: 30500381]
United States Department of Labor. Occupational Safety and Health Administration. Safety and Health Guides/Nerve Agents Guide. https://www.osha.gov/SLTC/emergencypreparedness/guides/nerve.html
CLONIDINE & OTHER SYMPATHOLYTIC ANTIHYPERTENSIVES
Overdosage with these agents (clonidine, guanabenz, guanfacine, methyldopa) causes bradycardia, hypotension, miosis, respiratory depression, and coma. (Transient hypertension occasionally occurs after acute overdosage, a result of peripheral alpha-adrenergic effects in high doses.) Symptoms are usually resolved in less than 24 hours, and deaths are rare. Similar symptoms may occur after ingestion of topical nasal decongestants chemically similar to clonidine (oxymetazoline, tetrahydrozoline, naphazoline). Brimonidine and apraclonidine are used as ophthalmic preparations for glaucoma. Tizanidine is a centrally acting muscle relaxant structurally related to clonidine; it produces similar toxicity in overdose.
 Treatment
Treatment
A. Emergency and Supportive Measures
Give activated charcoal. Maintain the airway and support respiration if necessary. Symptomatic treatment is usually sufficient even in massive overdose. Maintain blood pressure with intravenous fluids. Dopamine can also be used. Atropine is usually effective for bradycardia.
B. Specific Treatment
There is no specific antidote. Although tolazoline has been recommended for clonidine overdose, its effects are unpredictable and it should not be used. Naloxone has been reported to be successful in a few anecdotal and poorly substantiated cases.
Isbister GK et al. Adult clonidine overdose: prolonged bradycardia and central nervous system depression, but not severe toxicity. Clin Toxicol (Phila). 2017 Mar;55(3):187–92. [PMID: 28107093]
COCAINE
See Amphetamines & Cocaine.
CYANIDE
Cyanide is a highly toxic chemical used widely in research and commercial laboratories and many industries. Its gaseous form, hydrogen cyanide, is an important component of smoke in fires. Cyanide-generating glycosides are also found in the pits of apricots and other related plants. Cyanide is generated by the breakdown of nitroprusside, and poisoning can result from rapid high-dose infusions. Cyanide is also formed by metabolism of acetonitrile, a solvent found in some over-the-counter fingernail glue removers. Cyanide is rapidly absorbed by inhalation, skin absorption, or ingestion. It disrupts cellular function by inhibiting cytochrome oxidase and preventing cellular oxygen utilization.
 Clinical Findings
Clinical Findings
The onset of toxicity is nearly instantaneous after inhalation of hydrogen cyanide gas but may be delayed for minutes to hours after ingestion of cyanide salts or cyanogenic plants or chemicals. Effects include headache, dizziness, nausea, abdominal pain, and anxiety, followed by confusion, syncope, shock, seizures, coma, and death. The odor of “bitter almonds” may be detected on the victim’s breath or in vomitus, though this is not a reliable finding. The venous oxygen saturation may be elevated (greater than 90%) in severe poisonings because tissues have failed to take up arterial oxygen.
 Treatment
Treatment
A. Emergency and Supportive Measures
Remove the victim from exposure, taking care to avoid exposure to rescuers. For suspected cyanide poisoning due to nitroprusside infusion, stop or slow the rate of infusion. (Metabolic acidosis and other signs of cyanide poisoning usually clear rapidly.)
For cyanide ingestion, administer activated charcoal. Although charcoal has a low affinity for cyanide, the usual doses of 60–100 g are adequate to bind typically ingested lethal doses (100–200 mg).
B. Specific Treatment
In the United States, there are two available cyanide antidote regimens. The conventional cyanide antidote package (Nithiodote) contains sodium nitrite (to induce methemoglobinemia, which binds free cyanide) and sodium thiosulfate (to promote conversion of cyanide to the less toxic thiocyanate). Administer 3% sodium nitrite solution, 10 mL intravenously followed by 25% sodium thiosulfate solution, 50 mL intravenously (12.5 g). Caution: Nitrites may induce hypotension and dangerous levels of methemoglobin.
The other approved cyanide treatment in the United States is hydroxocobalamin (Cyanokit, EMD Pharmaceuticals), a newer and potentially safer antidote. The adult dose of hydroxocobalamin is 5 g intravenously (children’s dose is 70 mg/kg). Note: Hydroxocobalamin causes red discoloration of skin and body fluids that may last several days and can interfere with some laboratory tests.
Hendry-Hofer TB et al. A review on ingested cyanide: risks, clinical presentation, diagnostics, and treatment challenges. J Med Toxicol. 2019 Apr;15(2):128–33. [PMID: 30539383]
Parker-Cote JL et al. Challenges in the diagnosis of acute cyanide poisoning. Clin Toxicol (Phila). 2018 Jul;56(7):609–17. [PMID: 29417853]
DIETARY SUPPLEMENTS & HERBAL PRODUCTS
Unlike prescription and over-the-counter pharmaceuticals, dietary supplements do not require FDA approval, do not undergo the same premarketing evaluation of safety and efficacy as drugs, and purveyors may or may not adhere to good manufacturing practices and quality control standards. Supplements may cause illness as a result of intrinsic toxicity, misidentification or mislabeling, drug-herb reactions, or intentional adulteration with pharmaceuticals. If you suspect a dietary supplement or herbal product may be the cause of an otherwise unexplained illness, contact the FDA (1-888-463-6332) or the regional poison control center (1-800-222-1222), or consult the following online database: https://www.fda.gov/food/dietary-supplements.
Table 38–7 lists selected examples of clinical toxicity from some of these products.
Table 38–7. Examples of potential toxicity associated with some dietary supplements and herbal medicines.

Lim DY et al. Collective exposure to lead from an approved natural product-derived drug in Korea. Ann Occup Environ Med. 2019 Aug 26;31:e20. [PMID: 31620297]
Roytman MM et al. Botanicals and hepatotoxicity. Clin Pharmacol Ther. 2018 Sep;104(3):458–69. [PMID: 29920648]
Wong LL et al. Urgent liver transplantation for dietary supplements: an under-recognized problem. Transplant Proc. 2017 Mar;49(2):322–5. [PMID: 28219592]
DIGITALIS & OTHER CARDIAC GLYCOSIDES
Cardiac glycosides paralyze the Na+-K+-ATPase pump and have potent vagotonic effects. Intracellular effects include enhancement of calcium-dependent contractility and shortening of the action potential duration. A number of plants (eg, oleander, foxglove, lily-of-the-valley) contain cardiac glycosides. Bufotenin, a cardiotoxic steroid found in certain toad secretions and used as an herbal medicine and a purported aphrodisiac, has pharmacologic properties similar to cardiac glycosides.
 Clinical Findings
Clinical Findings
Intoxication may result from acute single exposure or chronic accidental overmedication, especially in patients with kidney dysfunction taking digoxin. After acute overdosage, nausea and vomiting, bradycardia, hyperkalemia, and AV block frequently occur. Patients in whom toxicity develops gradually during long-term therapy may be hypokalemic and hypomagnesemic owing to concurrent diuretic treatment and more commonly present with ventricular arrhythmias (eg, ectopy, bidirectional ventricular tachycardia, or ventricular fibrillation). Digoxin levels may be only slightly elevated in patients with intoxication from cardiac glycosides other than digoxin because of limited cross-reactivity of immunologic tests.
 Treatment
Treatment
A. Emergency and Supportive Measures
After acute ingestion, administer activated charcoal. Monitor potassium levels and cardiac rhythm closely. Treat bradycardia initially with atropine (0.5–2 mg intravenously) or a transcutaneous external cardiac pacemaker.
B. Specific Treatment
For patients with significant intoxication, administer digoxin-specific antibodies (digoxin immune Fab [ovine]; DigiFab). Estimation of the dose is based on the body burden of digoxin calculated from the ingested dose or the steady-state serum digoxin concentration, as described below. More effective binding of digoxin may be achieved if the dose is given partly as a bolus and the remainder as an infusion over a few hours.
1. From the ingested dose—Number of vials = approximately 1.5–2 × ingested dose (mg).
2. From the serum concentration—Number of vials = serum digoxin (ng/mL) × body weight (kg) × 10–2. Note: This is based on the equilibrium digoxin level; after acute overdose, serum levels may be falsely high for several hours before tissue distribution is complete, and overestimation of the DigiFab dose is likely.
3. Empiric dosing—Empiric titration of DigiFab may be used if the patient’s condition is relatively stable and an underlying condition (eg, atrial fibrillation) favors retaining a residual level of digitalis activity. Start with one or two vials and reassess the patient’s clinical condition after 20–30 minutes. For cardiac glycosides other than digoxin or digitoxin, there is no formula for estimation of vials needed and treatment is entirely based on response to empiric dosing.
Note: After administration of digoxin-specific Fab antibody fragments, serum digoxin levels may be falsely elevated depending on the assay technique.
Arbabian H et al. Elderly patients with suspected chronic digoxin toxicity: a comparison of clinical characteristics of patients receiving and not receiving digoxin-Fab. Emerg Med Australas. 2018 Apr;30(2):242–8. [PMID: 29316267]
ETHANOL, BENZODIAZEPINES, & OTHER SEDATIVE-HYPNOTIC AGENTS
The group of agents known as sedative-hypnotic drugs includes a variety of products used for the treatment of anxiety, depression, insomnia, and epilepsy. Besides common benzodiazepines, such as lorazepam, alprazolam, clonazepam, diazepam, oxazepam, chlordiazepoxide, and triazolam, this group includes the newer benzodiazepine-like hypnotics zolpidem, zopiclone, and zaleplon, the muscle relaxants baclofen and carisoprodol, and barbiturates such as phenobarbital. Ethanol and other selected agents are also popular recreational drugs. All of these drugs depress the central nervous system reticular activating system, cerebral cortex, and cerebellum.
 Clinical Findings
Clinical Findings
Mild intoxication produces euphoria, slurred speech, and ataxia. Ethanol intoxication may produce hypoglycemia, even at relatively low concentrations, in children and in fasting adults. With more severe intoxication, stupor, coma, and respiratory arrest may occur. Carisoprodol (Soma) commonly causes muscle jerking or myoclonus. Death or serious morbidity is usually the result of pulmonary aspiration of gastric contents. Bradycardia, hypotension, and hypothermia are common. Patients with massive intoxication may appear to be dead, with no reflex responses and even absent electroencephalographic activity. Diagnosis and assessment of severity of intoxication are usually based on clinical findings. Ethanol serum levels over 300 mg/dL (0.3 g/dL; 65 mmol/L) can produce coma in infrequent drinkers, while regular drinkers may remain awake at much higher levels.
 Treatment
Treatment
A. Emergency and Supportive Measures
Administer activated charcoal if the patient has ingested a massive dose and the airway is protected. Repeat-dose charcoal may enhance elimination of phenobarbital, but it has not been proved to improve clinical outcome. Hemodialysis may be necessary for patients with severe phenobarbital intoxication.
B. Specific Treatment
Flumazenil is a benzodiazepine receptor-specific antagonist; it has no effect on ethanol, barbiturates, or other sedative-hypnotic agents. If used, flumazenil is given slowly intravenously, 0.2 mg over 30–60 seconds, and repeated in 0.2–0.5 mg increments as needed up to a total dose of 3–5 mg. Caution: Flumazenil should rarely be used because it may induce seizures in patients with preexisting seizure disorder, benzodiazepine tolerance, or concomitant tricyclic antidepressant or other convulsant overdose. If seizures occur, diazepam and other benzodiazepine anticonvulsants will not be effective. As with naloxone, the duration of action of flumazenil is short (2–3 hours) and resedation may occur, requiring repeated doses.
Santos C et al. Sedative-hypnotic drug withdrawal syndrome: recognition and treatment. Emerg Med Pract. 2017 Mar;19(3):1–20. [PMID: 28186869]
GAMMA-HYDROXYBUTYRATE (GHB)
GHB is a popular drug of abuse. It originated as a short-acting general anesthetic and is occasionally used in the treatment of narcolepsy. It gained popularity among bodybuilders for its alleged growth hormone stimulation and found its way into social settings, where it is consumed as a liquid. It has been used to facilitate sexual assault (“date-rape” drug). Symptoms after ingestion include drowsiness and lethargy followed by coma with respiratory depression. Muscle twitching and seizures are sometimes observed. Recovery is usually rapid, with patients awakening within a few hours. Other related chemicals with similar effects include butanediol and gamma-butyrolactone (GBL). A prolonged withdrawal syndrome has been described in some heavy users.
 Treatment
Treatment
Monitor the airway and assist breathing if needed. There is no specific treatment. Most patients recover rapidly with supportive care. GHB withdrawal syndrome may require very large doses of benzodiazepines; baclofen has also been used.
Busardò FP et al. Interpreting γ-hydroxybutyrate concentrations for clinical and forensic purposes. Clin Toxicol (Phila). 2019 Mar;57(3):149–63. [PMID: 30307336]
Floyd CN et al. Baclofen in gamma-hydroxybutyrate withdrawal: patterns of use and online availability. Eur J Clin Pharmacol. 2018 Mar;74(3):349–56. [PMID: 29198063]
Miró Ò et al. Intoxication by gamma hydroxybutyrate and related analogues: clinical characteristics and comparison between pure intoxication and that combined with other substances of abuse. Toxicol Lett. 2017 Aug 5;277:84–91. [PMID: 28579487]
Santos C et al. Sedative-hypnotic drug withdrawal syndrome: recognition and treatment. Emerg Med Pract. 2017 Mar;19(3):1–20. [PMID: 28186869]
HYPOGLYCEMIC DRUGS
Medications used for diabetes mellitus include insulin, sulfonylureas and other insulin secretagogues, alpha-glucosidase inhibitors (acarbose, miglitol), biguanides (metformin), thiazolidinediones (pioglitazone, rosiglitazone), sodium glucose transporter (SGLT2) inhibitors, and peptide analogs (pramlintide, exenatide) or enhancers (sitagliptin) (see Chapter 27). Of these, insulin and the insulin secretagogues are the most likely to cause hypoglycemia. Metformin can cause lactic acidosis, especially in patients with impaired kidney function or after intentional drug overdose. Euglycemic diabetic ketoacidosis has been reported with SGLT2 use. Table 27–5 lists the duration of hypoglycemic effect of oral hypoglycemic agents and Table 27–6 the extent and duration of various types of insulins.
 Clinical Findings
Clinical Findings
Hypoglycemia may occur quickly after injection of short-acting insulins or may be delayed and prolonged, especially if a large amount has been injected into a single area, creating a “depot” effect. Hypoglycemia after sulfonylurea ingestion is usually apparent within a few hours but may be delayed several hours, especially if food or glucose-containing fluids have been given.
 Treatment
Treatment
Give sugar and carbohydrate-containing food or liquids by mouth, or intravenous dextrose if the patient is unable to swallow safely. For severe hypoglycemia, start with D50W, 50 mL intravenously (25 g dextrose); repeat, if needed. Follow up with dextrose-containing intravenous fluids (D5W or D10W) to maintain a blood glucose greater than 70–80 mg/dL.
For hypoglycemia caused by sulfonylureas and related insulin secretagogues, consider use of octreotide, a synthetic somatostatin analog that blocks pancreatic insulin release. A dose of 50–100 mcg octreotide subcutaneously every 6–12 hours can reduce the need for exogenous dextrose and prevent rebound hypoglycemia from excessive dextrose dosing.
Admit all patients with symptomatic hypoglycemia after sulfonylurea overdose. Observe asymptomatic overdose patients for at least 12 hours.
Consider hemodialysis for patients with metformin overdose accompanied by severe lactic acidosis (lactate greater than 20 mmol/L or pH < 7.0).
Razavi-Nematollahi L et al. Adverse effects of glycemia-lowering medications in type 2 diabetes. Curr Diab Rep. 2019 Nov 20;19(11):132. [PMID: 31748838]
Scheen AJ. Cardiovascular effects of new oral glucose-lowering agents: DPP-4 and SGLT-2 inhibitors. Circ Res. 2018 May 11;122(10):1439–59. [PMID: 29748368]
Ueda P et al. Sodium glucose cotransporter 2 inhibitors and risk of serious adverse events: nationwide register-based cohort study. BMJ. 2018 Nov 14;363:k4365. [PMID: 30429124]
ISONIAZID
INH is an antibiotic used mainly in the treatment and prevention of tuberculosis. It may cause hepatitis with long-term use, especially in alcoholic patients and elderly persons. It produces acute toxic effects by competing with pyridoxal 5-phosphate, resulting in lowered brain gamma-aminobutyric acid (GABA) levels. Acute ingestion of as little as 1.5–2 g of INH can cause toxicity, and severe poisoning is likely to occur after ingestion of more than 80–100 mg/kg.
 Clinical Findings
Clinical Findings
Confusion, slurred speech, and seizures may occur abruptly after acute overdose. Severe lactic acidosis—out of proportion to the severity of seizures—is probably due to inhibited metabolism of lactate. Peripheral neuropathy and acute hepatitis may occur with long-term use.
Diagnosis is based on a history of ingestion and the presence of severe acidosis associated with seizures. INH is not usually included in routine toxicologic screening, and serum levels are not readily available.
 Treatment
Treatment
A. Emergency and Supportive Measures
Seizures may require higher than usual doses of benzodiazepines (eg, lorazepam, 3–5 mg intravenously) or administration of pyridoxine as an antidote.
Administer activated charcoal after large recent ingestion, but with caution because of the risk of abrupt onset of seizures.
B. Specific Treatment
Pyridoxine (vitamin B6) is a specific antagonist of the acute toxic effects of INH and is usually successful in controlling convulsions that do not respond to benzodiazepines. Give 5 g intravenously over 1–2 minutes or, if the amount ingested is known, give a gram-for-gram equivalent amount of pyridoxine. Patients taking INH are usually given 25–50 mg of pyridoxine orally daily to help prevent neuropathy.
Glatstein M et al. Pyridoxine for the treatment of isoniazid-induced seizures in intentional ingestions: the experience of a national poison center. Am J Emerg Med. 2018 Oct;36(10):1775–8. [PMID: 29397257]
LEAD
Lead is used in a variety of industrial and commercial products, such as firearms ammunition, storage batteries, solders, paints, pottery, plumbing, and gasoline and is found in some traditional Hispanic and Ayurvedic ethnic medicines. Lead toxicity usually results from chronic repeated exposure and is rare after a single ingestion. Lead produces a variety of adverse effects on cellular function and primarily affects the nervous system, gastrointestinal tract, and hematopoietic system.
 Clinical Findings
Clinical Findings
Lead poisoning often goes undiagnosed initially because presenting symptoms and signs are nonspecific and exposure is not suspected. Common symptoms include colicky abdominal pain, constipation, headache, and irritability. Severe poisoning may cause coma and convulsions. Chronic intoxication can cause learning disorders (in children) and motor neuropathy (eg, wrist drop). Lead-containing bullet fragments in or near joint spaces can result in chronic lead toxicity.
Diagnosis is based on measurement of the blood lead level. Whole blood lead levels above 5 mcg/dL warrant public health investigation. Levels between 10 and 25 mcg/dL have been associated with impaired neurobehavioral development in children. Levels of 25–50 mcg/dL may be associated with headache, irritability, and subclinical neuropathy. Levels of 50–70 mcg/dL are associated with moderate toxicity, and levels greater than 70–100 mcg/dL are often associated with severe poisoning. Other laboratory findings of lead poisoning include microcytic anemia with basophilic stippling and elevated free erythrocyte protoporphyrin.
 Treatment
Treatment
A. Emergency and Supportive Measures
The most critical intervention in the treatment of lead poisoning is identification of and removal from the source of exposure. For patients with encephalopathy, maintain a patent airway and treat coma and convulsions as described at the beginning of this chapter.
For recent acute ingestion, if a large lead-containing object (eg, fishing weight) is still visible in the stomach on abdominal radiograph, whole bowel irrigation, endoscopy, or even surgical removal may be necessary to prevent subacute lead poisoning. (The acidic gastric contents may corrode the metal surface, enhancing lead absorption. Once the object passes into the small intestine, the risk of toxicity declines.)
B. Specific Treatment
The indications for chelation depend on the blood lead level and the patient’s clinical state. A medical toxicologist or regional poison control center (1-800-222-1222) should be consulted for advice about selection and use of these antidotes.
1. Severe toxicity—Patients with severe intoxication (encephalopathy or levels greater than 70–100 mcg/dL) should receive edetate calcium disodium (ethylenediaminetetraacetic acid, EDTA), 1500 mg/m2/kg/day (approximately 50 mg/kg/day) in four to six divided doses or as a continuous intravenous infusion. Most clinicians also add dimercaprol (BAL), 4–5 mg/kg intramuscularly every 4 hours for 5 days, for patients with encephalopathy.
2. Less severe toxicity—Patients with less severe symptoms and asymptomatic patients with blood lead levels between 55 and 69 mcg/dL may be treated with edetate calcium disodium alone in dosages as above. An oral chelator, succimer (DMSA), is available for use in patients with mild to moderate intoxication. The usual dose is 10 mg/kg orally every 8 hours for 5 days, then every 12 hours for 2 weeks.
Angelon-Gaetz KA et al. Lead in spices, herbal remedies, and ceremonial powders sampled from home investigations for children with elevated blood lead levels—North Carolina, 2011–2018. MMWR Morb Mortal Wkly Rep. 2018 Nov 23;67(46):1290–4. [PMID: 30462630]
Laidlaw MA et al. Lead exposure at firing ranges—a review. Environ Health. 2017 Apr 4;16(1):34. [PMID: 28376827]
Miracle VA. Lead poisoning in children and adults. Dimens Crit Care Nurs. 2017 Jan/Feb;36(1):71–3. [PMID: 27902665]
Reuben A. Childhood lead exposure and adult neurodegenerative disease. J Alzheimers Dis. 2018;64(1):17–42. [PMID: 29865081]
LITHIUM
Lithium is widely used for the treatment of bipolar depression and other psychiatric disorders. The only normal route of lithium elimination is via the kidney, so patients with acute or chronic kidney disorders are at risk for accumulation of lithium resulting in gradual onset (chronic) toxicity. Intoxication resulting from chronic accidental overmedication or kidney impairment is more common and usually more severe than that seen after acute oral overdose.
 Clinical Findings
Clinical Findings
Mild to moderate toxicity causes lethargy, confusion, tremor, ataxia, and slurred speech. This may progress to myoclonic jerking, delirium, coma, and convulsions. Recovery may be slow and incomplete following severe intoxication. Laboratory studies in patients with chronic intoxication often reveal an elevated serum creatinine and an elevated BUN/creatinine ratio due to underlying volume contraction. The white blood cell count is often elevated. ECG findings include T-wave flattening or inversion, and sometimes bradycardia or sinus node arrest. Nephrogenic diabetes insipidus can occur with overdose or with therapeutic doses. Dysfunction of the thyroid and parathyroid glands has also been described as a result of prolonged lithium exposure.
Lithium levels may be difficult to interpret. Lithium has a low toxic:therapeutic ratio, and chronic intoxication can be seen with levels only slightly above the therapeutic range (0.8–1.2 mEq/L). In contrast, patients with acute ingestion may have transiently very high levels (up to 10 mEq/L reported) without any symptoms before the lithium fully distributes into tissues. Note: Falsely high lithium levels (as high as 6–8 mEq/L) can be measured if a green-top blood specimen tube (containing lithium heparin) is used for blood collection.
 Treatment
Treatment
After acute oral overdose, consider gastric lavage or whole bowel irrigation to prevent systemic absorption (Note: lithium is not adsorbed by activated charcoal). In all patients, evaluate kidney function and volume status, and give intravenous saline-containing fluids as needed. Monitor serum lithium levels and seek assistance with their interpretation and the need for dialysis from a medical toxicologist or regional poison control center (1-800-222-1222). Consider hemodialysis if the patient is markedly symptomatic or if the serum lithium level exceeds 4–5 mEq/L, especially if kidney function is impaired. Continuous renal replacement therapy may be an effective alternative to hemodialysis.
Baird-Gunning J et al. Lithium poisoning. J Intensive Care Med. 2017 May;32(4):249–63. [PMID: 27516079]
King JD et al. Extracorporeal removal of poisons and toxins. Clin J Am Soc Nephrol. 2019 Sep 6;14(9):1408–15. [PMID: 31439539]
LSD & OTHER HALLUCINOGENS
A variety of substances—ranging from naturally occurring plants and mushrooms to synthetic substances such as phencyclidine (PCP), toluene and other solvents, dextromethorphan, and lysergic acid diethylamide (LSD)—are abused for their hallucinogenic properties. The mechanism of toxicity and the clinical effects vary for each substance.
Many hallucinogenic plants and mushrooms produce anticholinergic delirium, characterized by flushed skin, dry mucous membranes, dilated pupils, tachycardia, and urinary retention. Other plants and mushrooms may contain hallucinogenic indoles such as mescaline and LSD, which typically cause marked visual hallucinations and perceptual distortion, widely dilated pupils, and mild tachycardia. PCP, a dissociative anesthetic agent similar to ketamine, can produce fluctuating delirium and coma, often associated with vertical and horizontal nystagmus. Toluene and other hydrocarbon solvents (butane, trichloroethylene, “chemo,” etc) cause euphoria and delirium and may sensitize the myocardium to the effects of catecholamines, leading to fatal dysrhythmias. Other drugs used for their psychostimulant effects include synthetic cannabinoid receptor agonists, Salvia divinorum, synthetic tryptamines, and phenylethylamines, and mephedrone and related cathinone derivatives. See https://www.erowid.org/psychoactives/psychoactives.shtml for descriptions of various hallucinogenic substances.
 Treatment
Treatment
A. Emergency and Supportive Measures
Maintain a patent airway and assist respirations if necessary. Treat coma, hyperthermia, hypertension, and seizures as outlined at the beginning of this chapter. For recent large ingestions, consider giving activated charcoal orally or by gastric tube.
B. Specific Treatment
Patients with anticholinergic delirium may benefit from a dose of physostigmine, 0.5–1 mg intravenously, not to exceed 1 mg/min. Dysphoria, agitation, and psychosis associated with LSD or mescaline intoxication may respond to benzodiazepines (eg, lorazepam, 1–2 mg orally or intravenously) or haloperidol (2–5 mg intramuscularly or intravenously) or another antipsychotic drug (eg, olanzapine or ziprasidone). Monitor patients who have sniffed solvents for cardiac dysrhythmias (most commonly premature ventricular contractions, ventricular tachycardia, ventricular fibrillation); treatment with beta-blockers such as propranolol (1–5 mg intravenously) or esmolol (250–500 mcg/kg intravenously, then 50 mcg/kg/min by infusion) may be more effective than lidocaine or amiodarone.
Caffrey CR et al. When good times go bad: managing ‘legal high’ complications in the emergency department. Open Access Emerg Med. 2017 Dec 20;10:9–23. [PMID: 29302196]
MARIJUANA & SYNTHETIC CANNABINOIDS
Marijuana refers to the crushed dried leaves and flowers of the Cannabis plant. These dried leaves and flowers contain the psychoactive cannabinoid delta-9-tetrahydrocannabinal (THC), which binds to endogenous cannabinoid receptors. Marijuana is usually smoked in cigarettes or pipes but may also be added to a variety of foods, beverages, and candies. Resin from the plant may be dried and pressed into blocks called hashish, and solvents may be used to extract THC into highly concentrated oils (butane hash oil). THC has been used medically as an appetite stimulant, as an antiemetic, and in the treatment of a variety of medical conditions. It has now been legalized for both medical and recreational use in an increasing number of US states (https://disa.com/map-of-marijuana-legality-by-state). Toxicity is dose dependent but varies significantly by individual, prior experience, and degree of tolerance. Synthetic cannabinoids (“Spice,” “K2,” “Black Mamba”) are laboratory designed analogs of THC. They have become increasingly popular and are associated with a variety of adverse side effects, including seizures, kidney dysfunction, and serious neuropsychiatric symptoms.
 Clinical Findings
Clinical Findings
Onset of symptoms after smoking is usually rapid (minutes) with a duration of effect of approximately 2 hours. Symptoms may be delayed after ingestion and can result in prolonged intoxication (up to 8 hours). Mild intoxication may result in euphoria, palpitations, heightened sensory awareness, altered time perception, and sedation. More severe intoxication may result in anxiety, visual hallucinations, and acute paranoid psychosis. Physical findings include tachycardia, orthostatic hypotension, conjunctival injection, incoordination, slurred speech, and ataxia. Long-term heavy marijuana use is associated with recurrent nausea, abdominal pain and vomiting, termed the cannabinoid hyperemesis syndrome. Children may inadvertently be exposed to marijuana through the consumption of THC-containing candies or other foods. Children may experience more severe symptoms including stupor, coma, and seizures.
 Treatment
Treatment
A. Emergency and Supportive Measures
Treat anxiety and paranoia with simple reassurance and placement into a calming environment. Benzodiazepines such as lorazepam or diazepam may be used for more severe behavioral and psychomotor symptoms. Hypotension and sinus tachycardia should be treated with intravenous fluids.
B. Specific Treatment
There is no specific antidote currently available. Consider activated charcoal early after ingestion of large quantities. Topical capsaicin and haloperidol have been used with variable success for the treatment of acute vomiting in patients with cannabinoid hyperemesis syndrome.
Lucas CJ et al. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br J Clin Pharmacol. 2018 Nov;84(11):2477–82. [PMID: 30001569]
Pintori N et al. Synthetic cannabinoids: the hidden side of Spice drugs. Behav Pharmacol. 2017 Sep;28(6):400–19. [PMID: 28692429]
Richards JR et al. Unintentional cannabis ingestion in children: a systematic review. J Pediatr. 2017 Nov;190:142–52. [PMID: 28888560]
Wang GS et al. Common substances of abuse. Pediatr Rev. 2018 Aug;39(8):403–14. [PMID: 30068741]
MERCURY
Mercury poisoning may occur by ingestion of inorganic mercuric salts, organic mercury compounds, or inhalation of metallic mercury vapor. Ingestion of the mercuric salts causes a burning sensation in the throat, discoloration and edema of oral mucous membranes, abdominal pain, vomiting, bloody diarrhea, and shock. Direct nephrotoxicity causes acute kidney injury. Inhalation of high concentrations of metallic mercury vapor may cause acute fulminant chemical pneumonia. Chronic mercury poisoning causes weakness, ataxia, intention tremors, irritability, and depression. Exposure to alkyl (organic) mercury derivatives from highly contaminated fish or fungicides used on seeds has caused ataxia, tremors, convulsions, and catastrophic birth defects. Nearly all fish have some traces of mercury contamination; the US Environmental Protection Agency (EPA) advises consumers to avoid swordfish, shark, king mackerel, and tilefish because they contain higher levels. Fish and shellfish that are generally low in mercury content include shrimp, canned light tuna (not albacore “white” tuna), salmon, pollock, and catfish. Dental fillings composed of mercury amalgam pose a very small risk of chronic mercury poisoning and their removal is rarely justified. Some imported skin lightening creams contain toxic quantities of mercury.
 Treatment
Treatment
A. Acute Poisoning
There is no effective specific treatment for mercury vapor pneumonitis. Remove ingested mercuric salts by lavage and administer activated charcoal. For acute ingestion of mercuric salts, give dimercaprol (BAL) at once, as for arsenic poisoning. Unless the patient has severe gastroenteritis, consider succimer (DMSA), 10 mg/kg orally every 8 hours for 5 days and then every 12 hours for 2 weeks. Unithiol (DMPS) is a chelator that can be given orally or parenterally but is not commonly available in the United States; it can be obtained from some compounding pharmacies. Maintain urinary output. Treat oliguria and anuria if they occur.
B. Chronic Poisoning
Remove from exposure. Neurologic toxicity is not considered reversible with chelation, although some authors recommend a trial of succimer or unithiol (contact a regional poison center or medical toxicologist for advice).
Jackson AC. Chronic neurological disease due to methylmercury poisoning. Can J Neurol Sci. 2018 Nov;45(6):620–3. [PMID: 30278852]
Pelclova D et al. Is chelation therapy efficient for the treatment of intravenous metallic mercury intoxication? Basic Clin Pharmacol Toxicol. 2017 Jun;120(6):628–33. [PMID: 27911474]
METHANOL & ETHYLENE GLYCOL
Methanol (wood alcohol) is commonly found in a variety of products, including solvents, duplicating fluids, record cleaning solutions, and paint removers. It is sometimes ingested intentionally by alcoholic patients as a substitute for ethanol and may also be found as a contaminant in bootleg whiskey. Ethylene glycol is the major constituent in most antifreeze compounds. The toxicity of both agents is caused by metabolism to highly toxic organic acids—methanol to formic acid; ethylene glycol to glycolic and oxalic acids. Diethylene glycol is a nephrotoxic solvent that has been improperly substituted for glycerine in various liquid medications (cough syrup, teething medicine, acetaminophen), causing numerous deaths in Haiti, Panama, and Nigeria.
 Clinical Findings
Clinical Findings
Shortly after ingestion of methanol or ethylene glycol, patients usually appear “drunk.” The serum osmolality (measured by freezing point depression) is usually increased, but acidosis is often absent early. After several hours, metabolism to toxic organic acids leads to a severe anion gap metabolic acidosis, tachypnea, confusion, convulsions, and coma. Methanol intoxication frequently causes visual disturbances, while ethylene glycol often produces oxalate crystalluria and acute kidney injury. Note: Point-of-care analytical devices commonly used in the emergency department may falsely measure glycolic acid (a toxic metabolite of ethylene glycol) as lactic acid.
 Treatment
Treatment
A. Emergency and Supportive Measures
For patients presenting within 30–60 minutes after ingestion, empty the stomach by aspiration through a nasogastric tube. Charcoal is not very effective but should be administered if other poisons or drugs have also been ingested.
B. Specific Treatment
Patients with significant toxicity (manifested by severe metabolic acidosis, altered mental status, markedly elevated osmol gap, or evidence of end-organ toxicity) should undergo hemodialysis as soon as possible to remove the parent compound and the toxic metabolites. Treatment with folic acid, thiamine, and pyridoxine may enhance the breakdown of toxic metabolites.
Ethanol blocks metabolism of the parent compounds by competing for the enzyme alcohol dehydrogenase. Fomepizole (4-methylpyrazole; Antizol) blocks alcohol dehydrogenase and is much easier to use than ethanol. If started before onset of acidosis, fomepizole may be used as the sole treatment for ethylene glycol ingestion in some cases. A regional poison control center (1-800-222-1222) should be contacted for indications and dosing.
Gallagher N et al. The diagnosis and management of toxic alcohol poisoning in the emergency department: a review article. Adv J Emerg Med. 2019 May 22;3(3):e28. [PMID: 31410405]
Kraut JA et al. Toxic alcohols. N Engl J Med. 2018 Jan18;378(3):270–80. [PMID: 29342392]
Ng PCY et al. Toxic alcohol diagnosis and management: an emergency medicine review. Intern Emerg Med. 2018 Apr;13(3):375–83. [PMID: 29427181]
Pohanka M. Antidotes against methanol poisoning: a review. Mini Rev Med Chem. 2019;19(14):1126–33. [PMID: 30864518]
METHEMOGLOBINEMIA-INDUCING AGENTS
A large number of chemical agents are capable of oxidizing ferrous hemoglobin to its ferric state (methemoglobin), a form that cannot carry oxygen. Drugs and chemicals known to cause methemoglobinemia include benzocaine (a local anesthetic found in some topical anesthetic sprays and a variety of nonprescription products), aniline, propanil (an herbicide), nitrites, nitrogen oxide gases, nitrobenzene, dapsone, phenazopyridine (Pyridium), and many others. Dapsone has a long elimination half-life and may produce prolonged or recurrent methemoglobinemia. Amyl nitrite and isobutyl nitrite (“poppers”) are inhaled as sexual stimulants but can result in methemoglobinemia.
 Clinical Findings
Clinical Findings
Methemoglobinemia reduces oxygen-carrying capacity and may cause dizziness, nausea, headache, dyspnea, confusion, seizures, and coma. The severity of symptoms depends on the percentage of hemoglobin oxidized to methemoglobin; severe poisoning is usually present when methemoglobin fractions are greater than 40–50%. Even at low levels (15–20%), victims appear cyanotic because of the “chocolate brown” color of methemoglobin, but they have normal Po2 results on arterial blood gas determinations. Conventional pulse oximetry gives inaccurate oxygen saturation measurements; the reading is often between 85% and 90%. Severe metabolic acidosis may be present. Hemolysis may occur, especially in patients susceptible to oxidant stress (ie, those with glucose-6-phosphate dehydrogenase deficiency).
 Treatment
Treatment
A. Emergency and Supportive Measures
Administer high-flow oxygen. If the causative agent was recently ingested, administer activated charcoal. Repeat-dose activated charcoal may enhance dapsone elimination.
B. Specific Treatment
Methylene blue enhances the conversion of methemoglobin to hemoglobin by increasing the activity of the enzyme methemoglobin reductase. For symptomatic patients, administer 1–2 mg/kg (0.1–0.2 mL/kg of 1% solution) intravenously. The dose may be repeated once in 15–20 minutes if necessary. Patients with hereditary methemoglobin reductase deficiency or glucose-6-phosphate dehydrogenase deficiency may not respond to methylene blue treatment. In severe cases where methylene blue is not available or is not effective, exchange blood transfusion may be necessary.
Farkas AN. Methemoglobinemia due to antifreeze ingestion. N Engl J Med. 2017 Nov 16;377(20):1993–4. [PMID: 29141168]
Salim SA et al. Upward trend of dapsone-induced methemoglobinemia in renal transplant community. Clin Nephrol. 2017 Sep;88(9):156–61. [PMID: 28699887]
Sewell CR et al. A case report of benzocaine-induced methemoglobinemia. J Pharm Pract. 2017 Jan 1:897190017723211. [PMID: 28803519]
Siendones E et al. Cellular and molecular mechanisms of recessive hereditary methaemoglobinaemia type II. J Clin Med. 2018 Oct 10;7(10):E341. [PMID: 30309019]
MUSHROOMS
There are thousands of mushroom species that cause a variety of toxic effects. The most dangerous species of mushrooms are Amanita phalloides and related species, which contain potent cytotoxins (amatoxins). Ingestion of even a portion of one amatoxin-containing mushroom may be sufficient to cause death.
The characteristic pathologic finding in fatalities from amatoxin-containing mushroom poisoning is acute massive necrosis of the liver.
 Clinical Findings
Clinical Findings
Amatoxin-containing mushrooms typically cause a delayed onset (8–12 hours after ingestion) of severe abdominal cramps, vomiting and profuse diarrhea, followed in 1–2 days by acute kidney injury, hepatic necrosis, and hepatic encephalopathy. Cooking the mushrooms does not prevent poisoning.
Monomethylhydrazine poisoning (Gyromitra and Helvella species) is more common following ingestion of uncooked mushrooms, as the toxin is water-soluble. Vomiting, diarrhea, hepatic necrosis, convulsions, coma, and hemolysis may occur after a latent period of 8–12 hours.
 Treatment
Treatment
A. Emergency Measures
After the onset of symptoms, efforts to remove the toxic agent are probably useless, especially in cases of amatoxin or gyromitrin poisoning, where there is usually a delay of 8–12 hours or more before symptoms occur and patients seek medical attention. However, activated charcoal is recommended for any recent ingestion of an unidentified or potentially toxic mushroom. Administer intravenous fluids liberally to replace massive losses from vomiting and diarrhea; monitor central venous pressure, urinary output, and kidney function tests to help guide volume replacement.
B. Specific Treatment
A variety of purported antidotes (eg, thioctic acid, penicillin, corticosteroids) have been suggested for amatoxin-type mushroom poisoning, but controlled studies are lacking and experimental data in animals are equivocal. Aggressive fluid replacement for diarrhea and intensive supportive care for hepatic failure are the mainstays of treatment. Silymarin (silibinin), a derivative of milk thistle, is commonly used in Europe, but is currently commercially available in the United States only as an oral nutritional supplement. The European intravenous product (Legalon-SIL) can be obtained in the United States under an emergency IND provided by the FDA. Contact the regional poison control center (1-800-222-1222) for more information. Liver transplant may be the only hope for survival in gravely ill patients—contact a liver transplant center early.
Bonacini M et al. Features of patients with severe hepatitis due to mushroom poisoning and factors associated with outcome. Clin Gastroenterol Hepatol. 2017 May;15(5):776–9. [PMID: 28189696]
Diaz JH. Amatoxin-containing mushroom poisonings: species, toxidromes, treatments, and outcomes. Wilderness Environ Med. 2018 Mar;29(1):111–8. [PMID: 29325729]
Kim T et al. Predictors of poor outcomes in patients with wild mushroom-induced acute liver injury. World J Gastroenterol. 2017 Feb 21;23(7):1262–7. [PMID: 28275306]
White J et al. Mushroom poisoning: a proposed new clinical classification. Toxicon. 2019 Jan;157:53–65. [PMID: 30439442]
OPIATES & OPIOIDS
Prescription and illicit opiates and opioids (morphine, heroin, codeine, oxycodone, fentanyl, hydromorphone, etc) are popular drugs of misuse and abuse and the cause of frequent hospitalizations for overdose. These drugs have widely varying potencies and durations of action; for example, some of the illicit fentanyl derivatives are up to 2000 times more potent than morphine. In recent years, poisonings and fatalities have been reported due to the illicit use of fentanyl and the presence of fentanyl and its derivatives in counterfeit medications. All of these agents decrease central nervous system activity and sympathetic outflow by acting on opiate receptors in the brain. Tramadol is an analgesic that is unrelated chemically to the opioids but acts on opioid receptors. Buprenorphine is a partial agonist-antagonist opioid used for the outpatient treatment of opioid addiction (Table 5–6).
 Clinical Findings
Clinical Findings
Mild intoxication is characterized by euphoria, drowsiness, and constricted pupils. More severe intoxication may cause hypotension, bradycardia, hypothermia, coma, and respiratory arrest. Pulmonary edema may occur. Death is usually due to apnea or pulmonary aspiration of gastric contents. Methadone may cause QT interval prolongation and torsades de pointes. While the duration of effect for heroin is usually 3–5 hours, methadone intoxication may last for 48–72 hours or longer. Tramadol, dextromethorphan, and meperidine also occasionally cause seizures. With meperidine, the metabolite normeperidine is probably the cause of seizures and is most likely to accumulate with repeated dosing in patients with chronic kidney disease. Wound botulism has been associated with skin-popping, especially involving “black tar” heroin. Buprenorphine added to an opioid regimen may precipitate acute withdrawal symptoms. Many opioids, including fentanyl, tramadol, oxycodone, and methadone, are not detected on routine urine toxicology “opiate” screening.
 Treatment
Treatment
A. Emergency and Supportive Measures
Protect the airway and assist ventilation. Administer activated charcoal for recent large ingestions.
B. Specific Treatment
Naloxone is a specific opioid antagonist that can rapidly reverse signs of narcotic intoxication. Although it is structurally related to the opioids, it has no agonist effects of its own. If no intravenous access is available, administer naloxone 4 mg intranasally, otherwise administer 0.2–2 mg intravenously and repeat as needed to awaken the patient and maintain airway protective reflexes and spontaneous breathing. Very large doses (10–20 mg) may be required for patients intoxicated by some opioids (eg, codeine, fentanyl derivatives). Caution: The duration of effect of naloxone is only about 2–3 hours; repeated doses may be necessary for patients intoxicated by long-acting drugs such as methadone. Continuous observation for at least 3 hours after the last naloxone dose is mandatory.
Chou R et al. Management of suspected opioid overdose with naloxone in out-of-hospital settings: a systematic review. Ann Intern Med. 2017 Dec 19;167(12):867–75. [PMID: 29181532]
Drummer OH. Fatalities caused by novel opioids: a review. Forensic Sci Res. 2018 May 7;4(2):95–110. [PMID: 31304441]
Jones CM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA. 2018 May1;319(17):1819–21. [PMID: 29715347]
Srivastava A et al. Primary care management of opioid use disorders: abstinence, methadone, or buprenorphine-naloxone? Can Fam Physician. 2017 Mar;63(3):200–5. [PMID: 28292795]
PESTICIDES: CHOLINESTERASE INHIBITORS
Organophosphorus and carbamate insecticides (organophosphates: parathion, malathion, etc; carbamates: carbaryl, aldicarb, etc) are widely used in commercial agriculture and home gardening and have largely replaced older, more environmentally persistent organochlorine compounds such as DDT and chlordane. The organophosphates and carbamates—also called anticholinesterases because they inhibit the enzyme acetylcholinesterase—cause an increase in acetylcholine activity at nicotinic and muscarinic receptors and in the peripheral and central nervous system. There are a variety of chemical agents in this group, with widely varying potencies. Most of them are poorly water-soluble, are often formulated with an aromatic hydrocarbon solvent such as xylene and are well absorbed through intact skin. Most chemical warfare “nerve agents” (such as GA [tabun], GB [sarin], GD [soman], and VX) are organophosphates.
 Clinical Findings
Clinical Findings
Inhibition of cholinesterase results in abdominal cramps, diarrhea, vomiting, excessive salivation, sweating, lacrimation, miosis, wheezing and bronchorrhea, seizures, and skeletal muscle weakness. Initial tachycardia is usually followed by bradycardia. Profound skeletal muscle weakness, aggravated by excessive bronchial secretions and wheezing, may result in respiratory arrest and death. Symptoms and signs of poisoning may persist or recur over several days, especially with highly lipid-soluble agents such as fenthion or dimethoate.
The diagnosis should be suspected in patients who present with miosis, sweating, and diarrhea. Serum and red blood cell cholinesterase activity is usually depressed at least 50% below baseline in those victims who have severe intoxication.
 Treatment
Treatment
A. Emergency and Supportive Measures
If the agent was recently ingested, consider gut decontamination by aspiration of the liquid using a nasogastric tube followed by administration of activated charcoal. If the agent is on the victim’s skin or hair, wash repeatedly with soap or shampoo and water. Providers should take care to avoid skin exposure by wearing gloves and waterproof aprons. Dilute hypochlorite solution (eg, household bleach diluted 1:10) is reported to help break down organophosphate pesticides and nerve agents on equipment or clothing.
B. Specific Treatment
Atropine reverses excessive muscarinic stimulation and is effective for treatment of salivation, bronchial hypersecretion, wheezing, abdominal cramping, and sweating. However, it does not interact with nicotinic receptors at autonomic ganglia and at the neuromuscular junction and has no direct effect on muscle weakness. Administer 2 mg intravenously, and if there is no response after 5 minutes, give repeated boluses in rapidly escalating doses (eg, doubling the dose each time) as needed to dry bronchial secretions and decrease wheezing; as much as several hundred milligrams of atropine has been given to treat severe poisoning.
Pralidoxime (2-PAM, Protopam) is a more specific antidote that reverses organophosphate binding to the cholinesterase enzyme; therefore, it should be effective at the neuromuscular junction as well as other nicotinic and muscarinic sites. It is most likely to be clinically effective if started very soon after poisoning, to prevent permanent binding of the organophosphate to cholinesterase. However, clinical studies have yielded conflicting results regarding the effectiveness of pralidoxime in reducing mortality. Administer 1–2 g intravenously as a loading dose and begin a continuous infusion (200–500 mg/h, titrated to clinical response). Continue to give pralidoxime as long as there is any evidence of acetylcholine excess. Pralidoxime is of questionable benefit for carbamate poisoning, because carbamates have only a transitory effect on the cholinesterase enzyme. Other, unproven therapies for organophosphate poisoning include magnesium, sodium bicarbonate, clonidine, and extracorporeal removal.
Gorecki L et al. Progress in acetylcholinesterase reactivators and in the treatment of organophosphorus intoxication: a patent review (2006–2016). Expert Opin Ther Pat. 2017 Sep; 27(9):971–85. [PMID: 28569609]
Hulse EJ et al. Organophosphorus nerve agent poisoning: managing the poisoned patient. Br J Anaesth. 2019 Oct;123(4):457–63. [PMID: 31248646]
PETROLEUM DISTILLATES & SOLVENTS
Petroleum distillate toxicity may occur from inhalation of the vapor or as a result of pulmonary aspiration of the liquid during or after ingestion. Acute manifestations of aspiration pneumonitis are vomiting, coughing, and bronchopneumonia. Some hydrocarbons—ie, those with aromatic or halogenated subunits—can also cause severe systemic poisoning after oral ingestion. Hydrocarbons can also cause systemic intoxication by inhalation. Vertigo, muscular incoordination, irregular pulse, myoclonus, and seizures occur with serious poisoning and may be due to hypoxemia or the systemic effects of the agents. Chlorinated and fluorinated hydrocarbons (trichloroethylene, Freons, etc) and many other hydrocarbons can cause ventricular arrhythmias due to increased sensitivity of the myocardium to the effects of endogenous catecholamines.
 Treatment
Treatment
Remove the patient to fresh air. For simple aliphatic hydrocarbon ingestion, gastric emptying and activated charcoal are not recommended, but these procedures may be indicated if the preparation contains toxic solutes (eg, an insecticide) or is an aromatic or halogenated product. Observe the victim for 6–8 hours for signs of aspiration pneumonitis (cough, localized crackles or rhonchi, tachypnea, and infiltrates on chest radiograph). Corticosteroids are not recommended. If fever occurs, give a specific antibiotic only after identification of bacterial pathogens by laboratory studies. Because of the risk of arrhythmias, use bronchodilators with caution in patients with chlorinated or fluorinated solvent intoxication. If tachyarrhythmias occur, use esmolol intravenously 25–100 mcg/kg/min.
Chen X et al. Successful treatment of propafenone-induced cardiac arrest by calcium gluconate. Am J Emerg Med. 2017 Aug;35(8):1209.e1–2. [PMID: 28390833]
Jayanth SH et al. Glue sniffing. Med Leg J. 2017 Mar;85(1):38–42. [PMID: 27694447]
SALICYLATES
Salicylates (aspirin, methyl salicylate, bismuth subsalicylate, etc) are found in a variety of over-the-counter and prescription medications. Salicylates uncouple cellular oxidative phosphorylation, resulting in anaerobic metabolism and excessive production of lactic acid and heat, and they also interfere with several Krebs cycle enzymes. A single ingestion of more than 200 mg/kg of salicylate is likely to produce significant acute intoxication. Poisoning may also occur as a result of chronic excessive dosing over several days. Although the half-life of salicylate is 2–3 hours after small doses, it may increase to 20 hours or more in patients with intoxication.
 Clinical Findings
Clinical Findings
Acute ingestion often causes nausea and vomiting, occasionally with gastritis. Moderate intoxication is characterized by hyperpnea (deep and rapid breathing), tachycardia, tinnitus, and elevated anion gap metabolic acidosis. (A normal anion gap sometimes occurs due to salicylate interference with the chemistry analyzer, falsely raising the measured chloride.) Serious intoxication may result in agitation, confusion, coma, seizures, cardiovascular collapse, pulmonary edema, hyperthermia, and death. The prothrombin time is often elevated owing to salicylate-induced hypoprothrombinemia. Central nervous system intracellular glucose depletion can occur despite normal measured serum glucose levels.
Diagnosis of salicylate poisoning is suspected in any patient with metabolic acidosis and is confirmed by measuring the serum salicylate level. Patients with levels greater than 100 mg/dL (1000 mg/L or 7.2 mcmol/L) after an acute overdose are more likely to have severe poisoning. On the other hand, patients with subacute or chronic intoxication may suffer severe symptoms with levels of only 60–70 mg/dL (4.3–5 mcmol/L). The arterial blood gas typically reveals a respiratory alkalosis with an underlying metabolic acidosis.
 Treatment
Treatment
A. Emergency and Supportive Measures
Administer activated charcoal orally. Gastric lavage followed by administration of extra doses of activated charcoal may be needed in patients who ingest more than 10 g of aspirin. The desired ratio of charcoal to aspirin is about 10:1 by weight; while this cannot always be given as a single dose, it may be administered over the first 24 hours in divided doses every 2–4 hours along with whole bowel irrigation. Give glucose-containing fluids to reduce the risk of cerebral hypoglycemia. Treat metabolic acidosis with intravenous sodium bicarbonate. This is critical because acidosis (especially acidemia, pH < 7.40) promotes greater entry of salicylate into cells, worsening toxicity. Warning: Sudden and severe deterioration can occur after rapid sequence intubation and controlled ventilation if the pH is allowed to fall due to hypercarbia during the apneic period.
B. Specific Treatment
Alkalinization of the urine enhances renal salicylate excretion by trapping the salicylate anion in the urine. Add 100 mEq (two ampules) of sodium bicarbonate to 1 L of 5% dextrose in 0.2% saline, and infuse this solution intravenously at a rate of about 150–200 mL/h. Unless the patient is oliguric or hyperkalemic, add 20–30 mEq of potassium chloride to each liter of intravenous fluid. Patients who are volume-depleted often fail to produce an alkaline urine (paradoxical aciduria) unless potassium is given.
Hemodialysis may be lifesaving and is indicated for patients with severe metabolic acidosis, markedly altered mental status, or significantly elevated salicylate levels (eg, greater than 100–120 mg/dL [1000–1200 mg/L or 7.2–8.6 mcmol/L] after acute overdose or greater than 60–70 mg/dL [600–700 mg/L or 4.3–5 mcmol/L] with subacute or chronic intoxication).
Bowers D et al. Managing acute salicylate toxicity in the emergency department. Adv Emerg Nurs J. 2019 Jan/Mar;41(1):76–85. [PMID: 30702537]
McCabe DJ et al. The association of hemodialysis and survival in intubated salicylate-poisoned patients. Am J Emerg Med. 2017 Jun;35(6):899–903. [PMID: 28438446]
Shively RM et al. Acute salicylate poisoning: risk factors for severe outcome. Clin Toxicol (Phila). 2017 Mar;55(3):175–80. [PMID: 28064509]
SEAFOOD POISONINGS
A variety of intoxications may occur after eating certain types of fish or other seafood. These include scombroid, ciguatera, paralytic shellfish, and puffer fish poisoning. The mechanisms of toxicity and clinical presentations are described in Table 38–8. In the majority of cases, the seafood has a normal appearance and taste (scombroid may have a peppery taste).
Table 38–8. Common seafood poisonings.
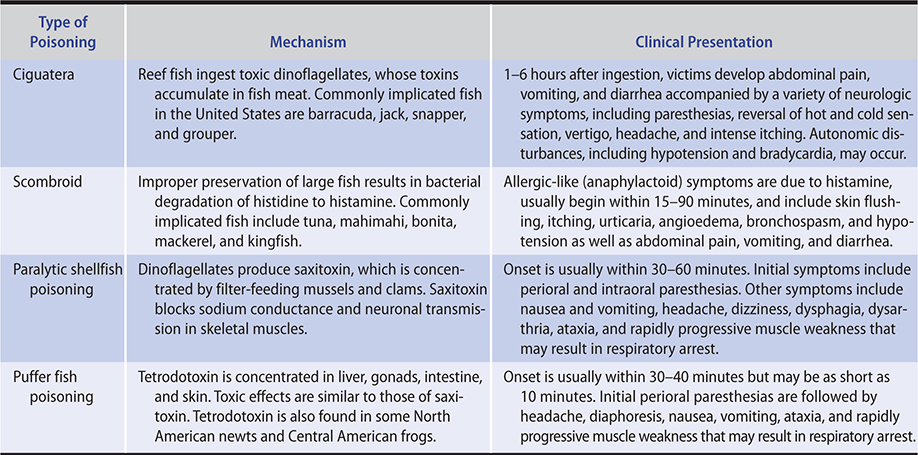
 Treatment
Treatment
A. Emergency and Supportive Measures
Caution: Abrupt respiratory arrest may occur in patients with acute paralytic shellfish and puffer fish poisoning. Observe patients for at least 4–6 hours. Replace fluid and electrolyte losses from gastroenteritis with intravenous saline or other crystalloid solution.
For recent ingestions, it may be possible to adsorb residual toxin in the gut with activated charcoal, 50–60 g orally.
B. Specific Treatment
There is no specific antidote for paralytic shellfish or puffer fish poisoning.
1. Ciguatera—There are anecdotal reports of successful treatment of acute neurologic symptoms with mannitol, 1 g/kg intravenously, but this approach is not widely accepted.
2. Scombroid—Antihistamines such as diphenhydramine, 25–50 mg intravenously, and the H2-blocker cimetidine, 300 mg intravenously, are usually effective.
Chinain M et al. Ciguatera poisoning in French Polynesia: insights into the novel trends of an ancient disease. New Microbes New Infect. 2019 Jun 7;31:100565. [PMID: 31312457]
Colombo FM et al. Histamine food poisonings: a systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2018 May 3;58(7):1131–51. [PMID: 27791395]
Mullins ME et al. Is mannitol the treatment of choice for patients with ciguatera fish poisoning? Clin Toxicol (Phila). 2017 Nov;55(9):947–55. [PMID: 28535116]
Warrell DA. Venomous bites, stings, and poisoning: an update. Infect Dis Clin North Am. 2019 Mar;33(1):17–38. [PMID: 30712761]
SNAKE BITES
The venom of poisonous snakes and lizards may be predominantly neurotoxic (coral snake) or predominantly cytolytic (rattlesnakes, other pit vipers). Neurotoxins cause respiratory paralysis; cytolytic venoms cause tissue destruction by digestion and hemorrhage due to hemolysis and destruction of the endothelial lining of the blood vessels. The manifestations of rattlesnake envenomation are mostly local pain, redness, swelling, and extravasation of blood. Perioral tingling, metallic taste, nausea and vomiting, hypotension, and coagulopathy may also occur. Thrombocytopenia can persist for several days after a rattlesnake bite. Neurotoxic envenomation may cause ptosis, dysphagia, diplopia, and respiratory arrest.
 Treatment
Treatment
A. Emergency Measures
Immobilize the patient and the bitten part in a neutral position. Avoid manipulation of the bitten area. Transport the patient to a medical facility for definitive treatment. Do not give alcoholic beverages or stimulants; do not apply ice; do not apply a tourniquet. The potential trauma to underlying tissues resulting from incision and suction performed by unskilled people is probably not justified in view of the small amount of venom that can be recovered.
B. Specific Antidote and General Measures
1. Pit viper (eg, rattlesnake) envenomation—There are two commercially available antivenins for rattlesnake envenomation (CroFab and Anavip). Depending on the severity of symptoms CroFab is administered in increments of 4–6 vials by slow intravenous drip in 250–500 mL saline. For more serious envenomation with marked local effects and systemic toxicity (eg, hypotension, coagulopathy), higher doses and additional vials may be required. The dosing of Anavip is 10 vials by slow intravenous infusion over 60 minutes initially followed by additional 10-vial increments as needed for more serious envenomations or for progression of symptoms. Monitor vital signs and the blood coagulation profile. Type and cross-match blood. The adequacy of venom neutralization is indicated by improvement in symptoms and signs, and the rate that swelling slows. Prophylactic antibiotics are not indicated after a rattlesnake bite.
2. Elapid (coral snake) envenomation—Give 1–2 vials of specific antivenom as soon as possible. Note: Pfizer/Wyeth no longer makes coral snake antivenom in the United States and remaining supplies are dwindling. To locate antisera for this or exotic snakes, call a regional poison control center (1-800-222-1222).
August JA et al. Prophylactic antibiotics are not needed following rattlesnake bites. Am J Med. 2018 Nov 131(11):1367–71. [PMID: 30392637]
Corbett B et al. North American snake envenomation. Emerg Med Clin North Am. 2017 May;35(2):339–54. [PMID: 28411931]
Gutiérrez JM et al. Unresolved issues in the understanding of the pathogenesis of local tissue damage induced by snake venoms. Toxicon. 2018 Jun 15;148:123–31. [PMID: 29698755]
Waiddyanatha S et al. Long-term effects of snake envenoming. Toxins (Basel). 2019 Mar 31;11(4):E193. [PMID: 30935096]
Warrell DA. Venomous bites, stings, and poisoning: an update. Infect Dis Clin North Am. 2019 Mar;33(1):17–38. [PMID: 30712761]
SPIDER BITES & SCORPION STINGS
Envenomation from most species of spiders in the United States causes only local pain, redness, and swelling. The more venomous black widow spiders (Latrodectus mactans) cause generalized muscular pains, muscle spasms, and rigidity. The brown recluse spider (Loxosceles reclusa) causes progressive local necrosis as well as hemolytic reactions (rare).
Stings by most scorpions in the United States cause only local pain. Stings by the more toxic Centruroides species (found in the southwestern United States) may cause muscle cramps, twitching and jerking, and occasionally hypertension, convulsions, and pulmonary edema. Stings by scorpions from other parts of the world are not discussed here.
 Treatment
Treatment
A. Black Widow Spider Bites
Pain may be relieved with parenteral opioids or muscle relaxants (eg, methocarbamol, 15 mg/kg). Calcium gluconate 10%, 0.1–0.2 mL/kg intravenously, may transiently relieve muscle rigidity, though its effectiveness is unproven. Latrodectus antivenom is possibly more effective, but because of concerns about acute hypersensitivity reactions (horse serum–derived), it is often reserved for very young or elderly patients or those who do not respond promptly to the above measures. Horse serum sensitivity testing is required. (Instruction and testing materials are included in the antivenin kit.)
B. Brown Recluse Spider Bites
Because bites occasionally progress to extensive local necrosis, some authorities recommend early excision of the bite site, whereas others use oral corticosteroids. Anecdotal reports have claimed success with dapsone and colchicine. All of these treatments remain of unproven.
C. Scorpion Stings
No specific treatment other than analgesics is required for envenomations by most scorpions found in the United States. An FDA-approved specific antivenom is available for Centruroides stings.
Erickson TB et al. Arthropod envenomation in North America. Emerg Med Clin North Am. 2017 May;35(2):355–75. [PMID: 28411932]
O’Connor AD et al. Severe bark scorpion envenomation in adults. Clin Toxicol (Phila). 2018 Mar;56(3):170–4. [PMID: 28753044]
Ryan NM et al. Treatments for latrodectism—a systematic review on their clinical effectiveness. Toxins (Basel). 2017 Apr 21;9(4):E148. [PMID: 28430165]
Warrell DA. Venomous bites, stings, and poisoning: an update. Infect Dis Clin North Am. 2019 Mar;33(1):17–38. [PMID: 30712761]
THEOPHYLLINE & CAFFEINE
Methylxanthines, including theophylline and caffeine, are nonselective adenosine receptor antagonists. In overdose, toxicity results from the release of endogenous catecholamines with beta-1- and beta-2-adrenergic stimulation. Theophylline may cause intoxication after an acute single overdose, or intoxication may occur as a result of chronic accidental repeated overmedication or reduced elimination resulting from hepatic dysfunction or interacting drug (eg, cimetidine, erythromycin). The usual serum half-life of theophylline is 4–6 hours, but this may increase to more than 20 hours after overdose. Caffeine in energy drinks or herbal or dietary supplement products can produce similar toxicity.
 Clinical Findings
Clinical Findings
Mild intoxication causes nausea, vomiting, tachycardia, and tremulousness. Severe intoxication is characterized by ventricular and supraventricular tachyarrhythmias, hypotension, and seizures. Status epilepticus is common and often intractable to the usual anticonvulsants. After acute overdose (but not chronic intoxication), hypokalemia, hyperglycemia, and metabolic acidosis are common. Seizures and other manifestations of toxicity may be delayed for several hours after acute ingestion, especially if a sustained-release preparation such as Theo-Dur was taken.
Diagnosis is based on measurement of the serum theophylline concentration. Seizures and hypotension are likely to develop in acute overdose patients with serum levels greater than 100 mg/L (555 mcmol/L). Serious toxicity may develop at lower levels (ie, 40–60 mg/L [222–333 mcmol/L]) in patients with chronic intoxication. Serum caffeine levels are not routinely available in clinical practice, but in a study of 51 fatal cases the median level was 180 mg/L (range 33–567 mg/L).
 Treatment
Treatment
A. Emergency and Supportive Measures
After acute ingestion, administer activated charcoal. Repeated doses of activated charcoal may enhance theophylline elimination by “gut dialysis.” Addition of whole bowel irrigation should be considered for large ingestions involving sustained-release preparations.
Hemodialysis is effective in removing theophylline and is indicated for patients with status epilepticus or markedly elevated serum theophylline levels (eg, greater than 100 mg/L [555 mcmol/L] after acute overdose or greater than 60 mg/L [333 mcmol/L] with chronic intoxication).
B. Specific Treatment
Treat seizures with benzodiazepines (lorazepam, 2–3 mg intravenously, or diazepam, 5–10 mg intravenously) or phenobarbital (10–15 mg/kg intravenously). Phenytoin is not effective. Hypotension and tachycardia—which are mediated through excessive beta-adrenergic stimulation—may respond to beta-blocker therapy even in low doses. Administer esmolol, 25–50 mcg/kg/min by intravenous infusion, or propranolol, 0.5–1 mg intravenously.
Aggelopoulou E et al. Atrial fibrillation and shock: unmasking theophylline toxicity. Med Princ Pract. 2018;27(4):387–91. [PMID: 29936503]
Andrade A et al. Dangerous mistake: an accidental caffeine overdose. BMJ Case Rep. 2018 Jun 8;2018. [PMID: 29884665]
Carreon CC et al. How to recognize caffeine overdose. Nursing. 2019 Apr;49(4):52–5. [PMID: 30893206]
Jones AW. Review of caffeine-related fatalities along with postmortem blood concentrations in 51 poisoning deaths. J Anal Toxicol. 2017 Apr 1;41(3):167–72. [PMID: 28334840]
Kato Y et al. Extracorporeal membrane oxygenation for hypokalemia and refractory ventricular fibrillation associated with caffeine intoxication. J Emerg Med. 2019 Nov 15. [Epub ahead of print] [PMID: 31740156]
Kohl BA et al. Acute intentional caffeine overdose treated preemptively with hemodialysis. Am J Emerg Med. 2020 Mar;38(3):692.e1–692.e3. [PMID: 31785982]
TRICYCLIC & OTHER ANTIDEPRESSANTS
Tricyclic and related cyclic antidepressants are among the most dangerous drugs involved in suicidal overdose. These drugs have anticholinergic and cardiac depressant properties (“quinidine-like” sodium channel blockade). Tricyclic antidepressants produce more marked membrane-depressant cardiotoxic effects than the phenothiazines.
Newer-generation antidepressants such as trazodone, fluoxetine, citalopram, paroxetine, sertraline, bupropion, venlafaxine, and fluvoxamine are not chemically related to the tricyclic antidepressant agents and, with the exception of bupropion, do not generally produce quinidine-like cardiotoxic effects. However, they may cause seizures in overdoses and they may cause serotonin syndrome.
 Clinical Findings
Clinical Findings
Signs of severe intoxication may occur abruptly and without warning within 30–60 minutes after acute tricyclic overdose. Anticholinergic effects include dilated pupils, tachycardia, dry mouth, flushed skin, muscle twitching, and decreased peristalsis. Quinidine-like cardiotoxic effects include QRS interval widening (greater than 0.12 s; Figure 38–2), ventricular arrhythmias, AV block, and hypotension. Rightward-axis deviation of the terminal 40 ms of the QRS has also been described. Prolongation of the QT interval and torsades de pointes have been reported with several of the newer antidepressants. Seizures and coma are common with severe intoxication. Life-threatening hyperthermia may result from status epilepticus and anticholinergic-induced impairment of sweating. Among newer agents, bupropion and venlafaxine have been associated with a greater risk of seizures.
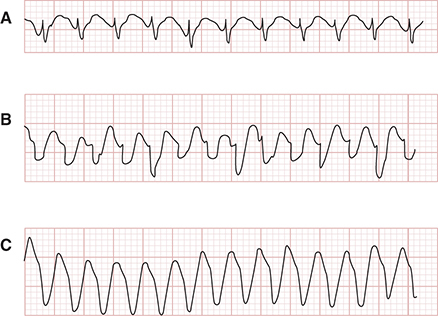
Figure 38–2. Cardiac arrhythmias resulting from tricyclic antidepressant overdose. A: Delayed intraventricular conduction results in prolonged QRS interval (0.18 s). B and C: Supraventricular tachycardia with progressive widening of QRS complexes mimics ventricular tachycardia. (Reproduced, with permission, from Benowitz NL, Goldschlager N. Cardiac disturbances in the toxicologic patient. In: Haddad LM, Winchester JF [editors], Clinical Management of Poisoning and Drug Overdose, 3rd edition. Saunders/Elsevier, 1998. Copyright © Elsevier.)
The diagnosis should be suspected in any overdose patient with anticholinergic side effects, especially if there is widening of the QRS interval or seizures. For intoxication by most tricyclic antidepressants, the QRS interval correlates with the severity of intoxication more reliably than the serum drug level.
Serotonin syndrome should be suspected if agitation, delirium, diaphoresis, tremor, hyperreflexia, clonus (spontaneous, inducible, or ocular), and fever develop in a patient taking serotonin reuptake inhibitors.
 Treatment
Treatment
A. Emergency and Supportive Measures
Observe patients for at least 6 hours and admit all patients with evidence of anticholinergic effects (eg, delirium, dilated pupils, tachycardia) or signs of cardiotoxicity.
Administer activated charcoal and consider gastric lavage after recent large ingestions. All of these drugs have large volumes of distribution and are not effectively removed by hemodialysis procedures.
B. Specific Treatment
Cardiotoxic sodium channel–depressant effects of tricyclic antidepressants may respond to boluses of sodium bicarbonate (50–100 mEq intravenously). Sodium bicarbonate provides a large sodium load that alleviates depression of the sodium-dependent channel. Reversal of acidosis may also have beneficial effects at this site. Maintain the pH between 7.45 and 7.50. Alkalinization does not promote excretion of tricyclic antidepressants. Prolongation of the QT interval or torsades de pointes is usually treated with intravenous magnesium or overdrive pacing. Severe cardiotoxicity in patients with overdoses of lipid-soluble drugs (eg, amitriptyline, bupropion) has reportedly responded to intravenous lipid emulsion (Intralipid), 1.5 mL/kg repeated one or two times if needed. Plasma exchange using albumin and ECMO have been reported successful in several cases.
Mild serotonin syndrome may be treated with benzodiazepines and withdrawal of the antidepressant. Moderate cases may respond to cyproheptadine (4 mg orally or via gastric tube hourly for three or four doses) or chlorpromazine (25 mg intravenously). Severe hyperthermia should be treated with neuromuscular paralysis and endotracheal intubation in addition to external cooling measures.
Bruccoleri RE et al. A literature review of the use of sodium bicarbonate for the treatment of QRS widening. J Med Toxicol. 2016 Mar;12(1):121–9. [PMID: 26159649]
Giwa A et al. The return of an old nemesis: survival after severe tricyclic antidepressant toxicity, a case report. Toxicol Rep. 2018 Mar 10;5:357–62. [PMID: 29854605]