Connective and skeletal tissues
Upper limb blood and lymphatic vessels
Important anatomical features of the upper limb
Lower limb blood and lymphatic vessels
Important anatomical features of the lower limb
Contents of the spinal canal and spinal nerves
• Connective tissues are broadly responsible for providing mechanical support, protection, and definition to other specialized tissue types. They include adipose tissue, tendons, aponeuroses, fascia, ligaments, and other fibrous and elastic tissues including parts of the haematopoietic system and the highly specialized tissues of cartilage and bone
• Significant differences exist between these tissue types, but each comprises a cellular component that is responsible for the production of an extracellular matrix of fibrous proteins and ground substance. In most connective tissue types, the extracellular matrix determines the mechanical properties of the tissue which are the result of its precise composition and arrangement
• In general, the fibrous components of connective tissue provide tensile strength, while the highly hydrated ground substance gives resistance to compression.
There are several different forms of connective tissue fibre. The type, concentration, and arrangement of these fibres are each important in determining the functional properties of different connective tissues.
• The most common fibrous protein is collagen, which is found in most types of connective tissue. This is a thick, strong, unbranched fibrous protein. There are many different types of collagen, each with different structural properties. The most abundant forms (e.g. types I and II) form fibrils with great tensile strength. The fibrils are formed from tropocollagen molecules, which consist of three peptide chains intertwined in a right-handed helix
• When stretched, elastic fibres return to their original size. These fibres are small, thin, and branching. In comparison to collagen, their tensile strength is low. They are abundant in the lungs, bladder, skin, and aorta, where they allow stretching without distortion or breaking of the tissue. They are formed in a three-stage process. Initially, a fibre comprised of fibrillin (a large molecule) and glycoproteins (called oxytalan) is formed. A protein called elastin is then deposited, through the oxytalan, in a disordered fashion to form elaunin. The third stage in this process involves the organization of elastin into the centre of fibril bundles to form elastic fibres
• Reticular fibres are thin fibres which are visible when stained with silver. They form a fragile network in the haematopoietic organs, spleen, liver, and lymph nodes. They filter blood and lymph and provide support for capillaries, muscle, and nerve cells.
Ground substance is the major ‘packing’ component of connective tissue and surrounds its cells and fibres.
• It consists of glycoproteins, glycosaminoglycans, and hyaluronic acid and forms an amorphous colourless, gel-like substance which is highly hydrated
• In cartilage and developing bone, the ground substance is mineralized by the deposition of calcium-containing crystals which leads to a marked alteration in its properties—particularly an increase in its strength.
• Fibroblasts, or similar specialized cells (e.g. osteoblasts and chondroblasts) are responsible for the synthesis and turnover of extracellular matrix and are usually the most abundant cell type found in connective tissue. They are flattened cells which, when active, are specialized for the production and secretion of proteins (e.g. collagen) and other macromolecules
• Fibrocytes are quiescent fibroblasts and are usually smaller with less prominent nuclei
• Adipose cells, which share some of the features of fibroblasts, are specialized for the storage of fat in connective tissue. Where adipose cells account for the majority of cells present, the tissue is referred to as adipose tissue, which frequently has an important cushioning role as well as providing thermal insulation. As histological sections, adipose cells appear empty because the fat is dissolved during the process of staining the slides. The nuclei are usually at the periphery of the cell with a tiny band of cytoplasm around the edge of the cell
• Macrophages and leucocytes are also present in connective tissue, as well as plasma cells which are produced from the bone marrow by lymphocytes. They migrate into the connective tissue, particularly in lymphatic or respiratory tissue where they play an important role in immune defence by secreting antibodies
• Mast cells are found in connective tissue, often associated with blood vessels. They are dark staining because they contain lots of histamine granules.
In addition to more specialized connective tissue types (e.g. cartilage and bone), there are two main types of connective tissue: loose and dense.
• Loose connective tissue comprises fibroblasts, collagen fibres, and macrophages. It is the more common of the two tissue types and is characterized by an abundance of ground substance and an irregular, loose structure of collagen fibres. Loose connective tissue is found around groups of muscle cells, blood vessels, and supporting epithelia
• Dense connective tissue has less ground substance and a more limited number of cell types, as it is densely packed with collagen fibres. These can be arranged regularly or irregularly and define the dense connective tissue as regular or irregular respectively, on the basis of the collagen fibre arrangement:
• Dense regular connective tissue is found in tendons and ligaments
• Dense irregular connective tissue is found in the capsules of organs the dermis of the skin, and where strong support is required. In tendons, collagen fibres are arranged in parallel bundles with fibroblasts arranged in rows between the densely packed bundles of fibres. This provides great tensile strength against forces pulling in a straight line.
• Cartilage covers and protects the articulating surfaces of bone as well as forming part of the septum of the nose, the external ear, and the embryological skeleton
• It can bear mechanical stress without permanent distortion and is an efficient shock absorber. It is made up of an extracellular matrix which is produced and maintained by specialized cells called chondrocytes and chondroblasts
• Chondroblasts are mesenchymal in origin and synthesize the extracellular matrix of cartilage. When these cells become surrounded by cartilage in lacunae they are called chondrocytes (mature cartilage cells), which maintain cartilage
• Cartilage is an avascular tissue which is surrounded by vascular connective tissue. Diffusion is the only means by which nutrients can enter and waste products leave.
There are three main types of cartilage, and the difference between them is the result of differences in composition of the extracellular matrix.
• Fibrocartilage has an irregular dense collagen fibre structure. It is formed of layers of thick collagen fibres and layers of cartilage matrix. It is found in the pubic symphysis and intervertebral discs
• Hyaline cartilage is the most common type of cartilage and contains abundant type II collagen fibres and large aggregating proteoglycan (aggrecan). It forms the basic structure of bones which then undergo endochondral ossification in the embryo. In adults, it forms part of the nose, larynx, trachea, and bronchi, and covers the articular surfaces of bones. Its smooth surface allows virtually friction-free movement at articulating joints
• Elastic cartilage contains more elastic fibres in its matrix and lines the walls of the auditory canal and forms part of the ear, the larynx, and the epiglottis.
• Bone is a rigid, tough structure which is important for support, load bearing, and protection. It provides for the attachment of muscles, storage of calcium and phosphate, and contains bone marrow which is important for haematopoiesis
• Bone consists of a cellular component as well as an extracellular matrix mineralized by the deposition of hydroxyapatite (basic calcium phosphate) and is a specialized type of connective tissue
• Osteogenic cells are derived from mesenchymal tissue and are undifferentiated, pluripotent stem cells with the capacity to produce bone-forming cells. The cells remain in the periosteum and endosteum in adults and are important for the remodelling, growth, and repair of bones by the provision of new osteoblasts when required
• Osteoblasts secrete osteoid—the organic component of bone. This is initially uncalcified, but rapidly becomes mineralized by the deposition of hydroxyapatite
• Osteoclasts are large, multinucleated cells which are important in bone remodelling because they resorb bone. They form Howship’s lacunae which are depressions of the bone surface where resorption has occurred
• Osteocytes are important in preserving the bone matrix. They sit in lacunae and are surrounded by the bony matrix
• Bone formation occurs through two different processes—intramembranous ossification and endochondral ossification. Intramembranous ossification occurs in bones such as the mandible, maxilla, clavicles, and most of the flat skull bones. It involves bone formation from a connective tissue matrix rather than from cartilage. The bone matrix is produced by osteoblasts. Endochondral ossification occurs in most of the rest of the bones of the body: this involves an initial hyaline cartilage structure that continues to grow. Gradually, cartilage is calcified by chondrocytes
• Osteoblasts are formed by osteoprogenitor cells which form an ossification centre within the bone. This is known as the primary ossification centre in the diaphysis (centre of the bone). Later, a secondary ossification centre forms at the epiphysis (swellings at the distal end of the cartilage framework). The epiphyseal plate region does not undergo mineralization until maturity, to allow long bone growth until adulthood. At the end of each long bone, a layer of articular cartilage covers the bone as part of the joint and comprises hyaline cartilage.
• Cancellous (spongy) bone comprises many interconnecting cavities. It forms the interior and epiphyses (the growth plate ends) of long bones
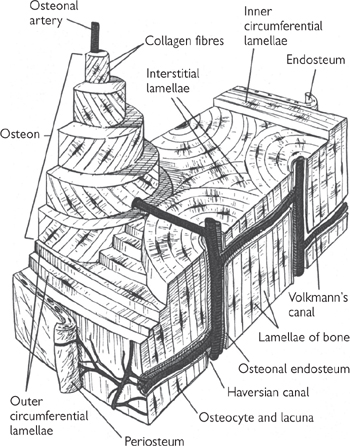
• This spongy bone is surrounded by an outer layer of compact bone which is much more dense (Fig. 5.1). This is much stronger and forms most of the outer layer of the bone shaft (the diaphysis)
• The bone marrow core of long bones is covered with a small amount of cancellous bone. In flat bones like those of the skull, bone forms with only a sliver of cancellous bone (diploë) sandwiched between the two plates of compact bone
• There are two types of bone: primary and secondary
• Primary bone comprises collagen fibres in an irregular arrangement, with a high number of osteocytes and little mineralization. This bone is usually replaced by secondary bone tissue in adults. In adults, it is only found in a few places (e.g. tooth sockets)
• Secondary bone is formed as the Haversian system (or osteon). This structure is found in most adult bone. Collagen fibres are arranged in lamellae (rows). These are often arranged around a central canal in a concentric fashion. The central canal contains the neurovascular bundle and loose connective tissue. This canal is known as the Haversian canal. Osteocytes are found between the concentric layers of lamellae in lacunae
• Mineralization of bone prevents the diffusion of nutrients. Instead, canaliculi (channels within the bone which contain extracellular fluid) allow efficient exchange of nutrients and waste products. Osteocytes in lacunae extend their cytoplasmic processes into the canaliculi, thereby allowing communication between osteocytes and nutrient uptake from the blood
• Bone remodelling is a continuous process. This characteristic is particularly important during growth and fracture healing. Remodelling enables the shape of the bone to be maintained as it grows.
Fig. 5.1 Diagram of a section of compact bone removed from the shaft of a long bone.
Reproduced with permission from Ross MH, Kaye GI, Pawlina W (2003). Histology: A Text and Atlas, 4th edn. Baltimore: Lippincott, Williams and Wilkins.
• Skin is a large organ that almost completely covers the exterior surfaces of the body. It comprises a specialized epithelium which includes various glands (e.g. sweat glands, sebaceous glands, mammary glands) and associated supporting tissues
• Skin has a number of important functions including protection of the body from damaging external agents (water, infection, sunlight), detection of sensory stimuli, thermoregulation, and prevention of dehydration
• Skin is arranged as a number of layers including the epidermis (outermost layer), dermis, and subcutaneous tissue (hypodermis). The relative thickness and structure of each of these layers is dependent on the area of the body and relates to specific functional specializations.
• The epidermis is the surface layer of skin cells in contact with the outside world. Sweat glands and hair follicles are downgrowths of this layer
• It is a stratified epithelium with a tough keratinized upper layer. It is formed from keratin-producing cells (keratinocytes) which die, forming keratin plates (squames). The outermost layer of keratin is constantly being shed and replaced by new keratinocytes from deeper layers
• The epidermis is divided into distinct layers:
• Stratum basale (basal layer): This layer sits on the basement membrane which separates the supporting dermis from the epidermis and is responsible for keratinocyte production. The cells are cuboidal or columnar and are attached to each other and to the underlying basement membrane. These cells are rich in ribosomes and mitochondria enabling rapid cell turnover and protein synthesis. Melanin granules are also present in pigmented skin
• Stratum spinosum (prickle layer): This layer, which sits on the basal layer, is formed from polyhedral cells with round central nuclei. A system of intercellular bridges made of cytoplasmic projections connect these prickle cells. These projections terminate as desmosomal junctions on the cell surface
• Stratum granulosum (granular layer): In this layer, the cells contain abundant keratohyaline granules. In the upper layers, cells become flattened and densely packed, with little cytosol
• Stratum lucidum: This layer merges with the upper layers of the stratum granulosum and consists of extremely flattened cells in which organelles and nuclei are not readily apparent
• Stratum corneum: The uppermost layers of the epidermis in which keratin is formed from dead cells. The waterproofing effect of this layer is a result of the hydrophobic properties of glycophospholipids, which have a glue-like effect, sticking the dead flakes of cells together. This can be washed away as shown by the wrinkling of the skin of the hands after extended exposure to water
• There is a constant need to replenish the epidermis, as the outer surface is constantly being sloughed off. Turnover of cells from basal cells to desquamated keratin varies from site to site in the body, with traumatized sites having a faster turnover (e.g. soles of the feet: ~25 days; the back: ~45 days)
• Skin can be classified according to whether the epidermis is thin or thick. Thick skin has a much deeper stratum corneum, stratum granulosum, and stratum lucidum. It is found in areas which are most exposed to abrasive forces (e.g. palms of the hands, soles of the feet).
• Melanocytes produce the skin pigment melanin, which is responsible for skin colouring and reduces damage caused by ultra-violet radiation. They are located in the basal layer. They synthesize melanin in cytoplasmic membrane-bound granules. These granules advance along cytoplasmic processes into the cytoplasm of basal and prickle layer keratinocytes
• Langherhan’s cells present phagocytosed antigenic material to lymphocytes. These cells possess cytoplasmic processes which increase the surface area of the cell membrane. Langherhan’s cells are found in all skin layers, but are most frequently seen in the prickle layer of the skin. In inflamed skin, the number of the cytoplasmic processes increases, especially during autoimmune or allergy-related skin disorders
• Merkel’s cells are sensory receptors in the skin and synapse with peripheral nerve endings. They are found as solitary cells or grouped together to form touch receptors where they are related to hair discs. They contain neuroendocrine granules.
• The basement membrane comprises three layers and separates the epidermal layer from the underlying dermis
• Basal cells are attached to the outermost layer—the lamina densa—and from here, anchoring proteins cross to the lamina lucida
• Fibronectin is abundant in the zone below the lamina densa (fibroreticular lamina)
• The lower surface of the lamina densa is attached to collagen fibres in the papillary dermis by fibrils made of type VII collagen.
• The dermo-epidermal junction binds the dermis and the epidermis together. Tethering fibres pass between the two layers and the intervening basement membrane
• The rete system is a series of downgrowths of the epidermis into the dermis which increases the area of attachment between the two layers. This is minimal over the back and more extensive over the fingertips and soles where shearing forces are increased.
• The middle layer of skin, the dermis, includes blood vessels, lymphatics, nerves and nerve endings, and epidermal appendages. These structures are embedded in a connective tissue stroma that is produced by fibroblasts
• The dermis consists of two layers:
• The superficial loose papillary dermis, a thin layer of loosely arranged collagen and elastin fibres, containing small capillary-sized blood vessels, fine nerves, and nerve endings
• The dense reticular dermis, which contains mainly collagen and elastic fibres. The reticular dermis is thicker, forming the bulk of the dermis. It contains blood vessels, nerves, and lymphatics supplying the skin and comprises dense bands of collagen and long, thick fibres of elastin. These generally run parallel with the skin
• The dermis contains two vascular plexuses—a deep plexus in the lower reticular dermis close to the border with the subcutis and a superficial plexus in the upper reticular dermis close to the junction with the papillary dermis
• Variations in blood flow within the dermis allow the skin to participate in thermoregulation. This is controlled by the many arteriovenous anastomoses within the dermis, including the glomus bodies. Loops from the superficial plexus extend upwards to the papillary dermis to form capillaries near the basement membrane of the epidermis.
There are four major specialized nerve endings detecting cutaneous sensation in skin:
• Free nerve endings detect pain, itch, and temperature and can be myelinated or unmyelinated
• Meissner’s corpuscles detect touch, are found mainly on the hands and feet, and have ordered nerve endings which are confined to dermal papillae
• Merkel’s cells are slow adapting touch receptors
• Pacinian corpuscles detect pressure and vibration and are encapsulated nerve endings with a characteristic structure. They are found mainly in deep dermis and subcutaneous fat on palms and soles.
The nerve supply to the skin consists of a sympathetic supply of unmyelinated nerves which control skin appendages (e.g. sweat glands) and vascular flow.
The subcutis is the deepest layer of skin and varies in size over the body. Adipose tissue forms the majority of this layer. It contains a network of arteries and veins which extend upwards into the dermo-subcutaneous junction, forming a cutaneous plexus.
The autonomic nervous system (see ‘synoptic transmission’, Chapter 4) controls the secretion of sweat from eccrine sweat glands. The secretory component is found in the subcutis or deep dermis and ducts communicate with the exterior. These ducts are coiled in the deep dermis and epidermal layers with straight connections between them. Apocrine glands are stimulated during the fight-or-flight response. They are downgrowths of the epidermis with unknown function. They are concentrated in the genito-anal region and axilla.
• Hair grows from hair follicles, which are invaginations of epidermal tissue. A bulbous expansion at the lower end of the hair follicle (Fig. 5.2) is called the hair bulb where specialized dermis forms the hair papilla
• Hair follicles are well supplied with small blood vessels and nerve endings
• Hair is formed of organized keratin. The hair follicle and shaft are controlled by the erector pili muscle which allows hair to stand on end
• Sebaceous glands around the follicle secrete sebum—a mixture of lipids
• Fingernails and toenails are hard plates of keratinized epithelium.
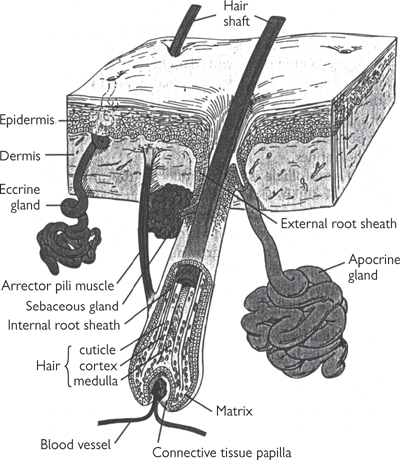
Fig. 5.2 Hair follicle and other skin appendages.
Reproduced with permission from Ross MH, Kaye GI, Pawlina W (2003). Histology: A Text and Atlas, 4th edn. Baltimore: Lippincott, Williams and Wilkins.
Comprises the collar bone (or clavicle) and the shoulder blade (or scapula). Together, they provide a mobile base to attach the upper limbs to the trunk.
The clavicle:
• Acts as a strut to distance the scapula and upper limb from the chest wall
• Forms articulations with the sternum and with the acromion of the scapula
• Transmits forces to the axial skeleton (fractures frequently result from falls on the outstretched arm)
• Lacks marrow and ossifies in membrane.
The triangular scapula:
• Articulates with the humerus at the glenoid fossa
• Possesses a prominent ridge on the posterior surface: the spine
• Provides large, flat surfaces and roughened processes for muscle attachments
• Maintains a strong purchase on the chest wall.
Comprise the bone of the upper arm (the humerus), the bones of the forearm (the radius), and the ulna.
The humerus:
• Acts as a mobile lever to direct forearm movement in any direction
• Consists of a head (in the shape of a half-sphere which articulates with the scapula) together with a neck and a shaft
• Articulates with the radius at the rounded capitulum
• Articulates with the ulna at the trochlea (the trochlea projects further at its medial border than at its lateral border, angling the forearm laterally with respect to the upper arm—this accounts for the carrying angle)
• Is often fractured at the ‘surgical neck’, below the anatomical head at the start of the shaft.
The radius:
• Possesses a head (proximal end), neck, and shaft
• Head is a thick, disc-like shape which articulates with the humerus
• Articulates with the scaphoid and lunate carpal bones at its distal end
• Is expanded at its distal end with an ulnar notch
• Is often fractured by a fall on an outstretched hand (a ‘Colles fracture’).
The ulna:
• Is not directly a part of the wrist joint
• Possesses a head (distal end), neck, and shaft
• Articulates with the humerus at the crescent-shaped trochlear notch
• Possesses a beak-shaped process (the olecranon) at its proximal extremity which, in combination with the humerus, locks the extended elbow joint to prevent overextension
• Articulates with the radius head at the radial notch.
Fig. 5.3 Bones of shoulder girdle and upper limb; anterior view.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p46 (Oxford, 2005). With permission of OUP.
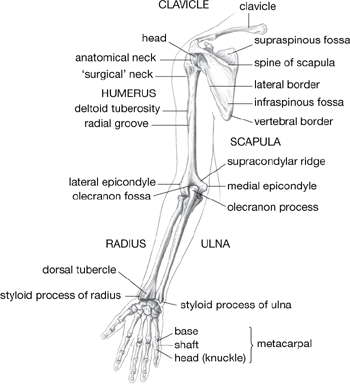
Fig. 5.4 Bones of shoulder girdle and limb; posterior view.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p46 (Oxford, 2005). With permission of OUP.
Comprise eight small bones of the wrist (the carpus, Fig. 5.5) and 19 bones of the fingers (the metacarpals and phalanges).
The carpus bones:
• Are distal to the wrist joint
• Are pebble-like and arranged in two rows of four:
• Scaphoid, lunate, triquetral, pisiform (a sesamoid bone) in proximal row
• Trapezium, trapezoid, capitate, hamate in distal row
• Are transversely arched, creating a hollow
• Provide a flexible but firm basis on which muscles can exert their action
• Articulate distally with the metacarpal bones.
The scaphoid is prone to fracture through fall on the outstretched hand.
The metacarpal bones:
• The first is the bony support for the base of the thumb
• The remaining four provide the framework for the palm of the hand
• Comprise a head, neck, and shaft
• Articulate distally with the first row of phalanges
• Are relatively immobile; only that of the thumb is truly mobile.
The phalanges:
• Are the bones of the fingers and thumb—there are three in each finger, two only in the thumb
• Comprise a base, shaft, and head
• Of the fingers are designated proximal, middle, distal
• Function as a unit, rather than as individual bones.
Fig. 5.5 Carpal bones; anterior view. Scaphoid (S), with its tubercle (t), waist, and proximal pole, lunate (L), triquetral (T), pisiform (a sesamoid bone) (P); distal row: trapezium (Tm), with its groove (g) and ridge (r), trapezoid (Td), capitate (C), hamate (H), and its hook (h).
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p46 (Oxford, 2005). With permission of OUP.
• Between medial end of clavicle and upper lateral edge of manubrium of sternum
• Atypical synovial joint—surfaces covered by fibrocartilage
• Synovial capsule encloses joint—reinforced by anterior and posterior sternoclavicular ligaments, costoclavicular ligament
• Fibrocartilaginous disc attaches to capsule; divides the joint into two cavities
• Between lateral end of clavicle and medial edge of acromion of scapula
• Stabilized mostly by coracoclavicular and acromioclavicular ligaments.
These joints transmit little of the force associated with upper limb movements, so dislocation is uncommon.
• Glenohumeral joint—between glenoid fossa of scapula and head of humerus
• Freely mobile, ball-and-socket synovial joint
• Encapsulated—synovial capsule is thin and loose inferiorly to permit wide range of movement
• Contains the glenoid labrum—rim of fibrocartilage attached to cavity margins
• Capsule strengthened by tendons of the rotator cuff
• Three glenohumeral ligaments, together with coracohumeral ligament, add stability.
• Trochlea of humerus and trochlear notch of ulna
• Capitulum of humerus and head of radius
• Head of radius and radial notch (the superior or proximal radio-ulnar joint)
• Capsule envelops all these articulations
• Capsule reinforced by lateral and medial ligaments (the radial and ulnar collateral ligaments)
• Superior radio-ulnar joint held together by annular ligament—permits rotation of radial head on ulna
• Posterior dislocation by a fall on outstretched hand.
Fig. 5.6 Bones and ligaments of the shoulder girdle.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p54 (Oxford, 2005). With permission of OUP.
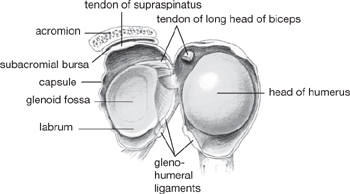
Fig. 5.7 Interior of shoulder joint.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p60 (Oxford, 2005). With permission of OUP.
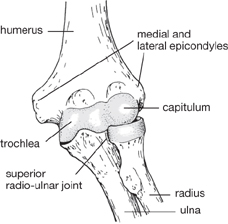
Fig. 5.8 Articular surfaces of elbow joint (anterior aspect).
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p70 (Oxford, 2005). With permission of OUP.
• Proximal and distal radio-ulnar joints (Fig. 5.9)
 Proximal: between head of radius with radial notch of ulna (see elbow)
Proximal: between head of radius with radial notch of ulna (see elbow)
 Distal: between ulnar notch of radius and head of ulna
Distal: between ulnar notch of radius and head of ulna
• A triangle of fibrocartilage (intra-articular disc) unites radius and ulna
• Shafts of radius and ulna joined by fibrous sheet—the interosseous membrane
• Distal end of radius and intra-articular disc articulate with proximal row of carpal bones
• Capsule strengthened by radial and ulnar collateral ligaments and by dorsal and palmar ligaments
• Flexor retinaculum bridges the concavity of the carpal bones, retains flexor tendons; runs from scaphoid, trapezium to pisiform and hook of hamate
• Protective palmar aponeurosis from tendon of palmaris longus merges with the flexor retinaculum
• Thinner extensor retinaculum across the back of the wrist from pisiform, hook of hamate to radius; it bridges grooves on dorsal aspect of lower radius into channels for extensor tendons.
• Adjacent carpal bones articulate at plane synovial joints to effect small sliding movements
• Significant movement can occur at the mid-carpal joints between carpal bones in the proximal and distal rows
• The thumb joint (1st carpo-metacarpal joint) is the most important
• Articulation between trapezium and 1st metacarpal
• This is a synovial saddle joint, which allows opposition of the thumb
• Condylar synovial joints allowing side-to-side movements
• Collateral ligaments between metacarpal and proximal phalanx
Fig. 5.9 Capsule and ligaments of the radio-ulnar joints.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p78 (Oxford, 2005). With permission of OUP.
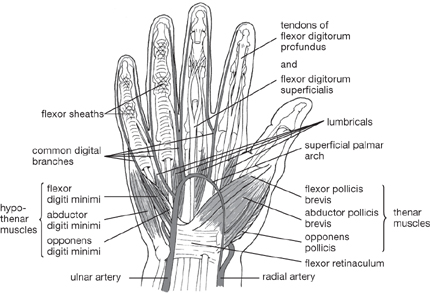
Fig. 5.10 Superficial aspect of palm.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p91 (Oxford, 2005). With permission of OUP.
Nerve supply is indicated by superscript. See Figures 5.11 and 5.12 for terms denoting position and movement of the body.
• Protraction (forward rotation)
• Serratus anteriorlong thoracic nerve
• Pectoralis minormedial pectoral nerve
• Retraction (backward rotation or bracing)
• Rhomboideus major and minor nerve to rhomboids
• Trapeziusspinal accessory nerve
• Levator scapulaedorsal scapular nerve, cervical roots
• Pectoralis major (clavicular head)pectoral nerves
• Deltoid (anterior)axillary nerve
• Coracobrachialismusculocutaneous nerve
• Bicepsmusculocutaneous nerve
• Extension (backward swinging)
• Latissimus dorsithoracodorsal nerve
• Triceps (long head)radial nerve
• Abduction (sideways movement away from the body)
• Supraspinatus (<15°)suprascapular nerve
• Serratus anterior and trapezius (>90°)
• Adduction (movement towards the body, across the chest)
• Teres majorlower subscapular nerve
• Infraspinatussuprascapular nerve
• A combination of all of the above.
• Brachialismusculocutaneous nerve
• Pronation (palm turned down)
• Pronator teres and quadratusmedian nerve
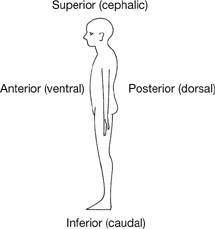
Fig. 5.11 Anatomical terms denoting position.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p3 (Oxford, 2005). With permission of OUP.
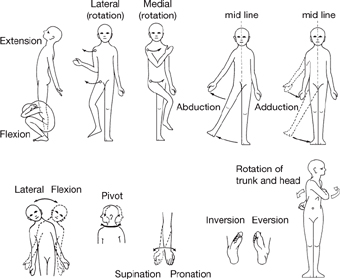
Fig. 5.12 Movement of the body.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p4 (Oxford, 2005). With permission of OUP.
• Palmar flexion (wrist dropped)
• Flexor carpi radialismedian nerve
• Flexor carpi ulnarisulnar nerve
• Extension (or dorsiflexion—wrist bent backwards)
• Extensor carpi radialisradial nerve
• Extensor carpi ulnarisradial nerve
• Abduction (radial deviation)
• Long flexor and extensor of the thumb
• a combination of all the above.
• Flexor digitorum superficialismedian nerve
• Flexor digitorum profundusmedian, ulnar nerves
• Lumbrical musclesmedian, ulnar nerves
• Extensor digitorum, indicis and minimiradial nerve
• Dorsal interosseiulnar nerve
• Palmar interosseiulnar nerve
• Hypothenar eminenceulnar nerve
 Abductor, flexor, and opponens digiti minimi
Abductor, flexor, and opponens digiti minimi
 Abductor, flexor pollicis brevis, and opponens pollicis
Abductor, flexor pollicis brevis, and opponens pollicis
• Abductor and extensor pollicis longusradial nerve.
Fig. 5.13 Movements of the fingers and thumb.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p89 (Oxford, 2005). With permission of OUP.
• Muscles connect vertebrae to the upper limb:
• Muscles connect the thoracic wall to the upper limb:
• To draw the upper limb forward, inward
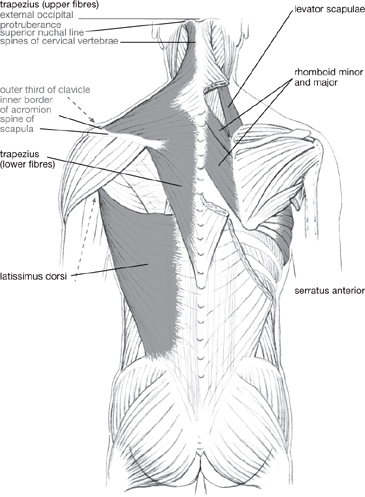
Fig. 5.14 Superficial muscles of the shoulder girdle and back.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p55 (Oxford, 2005). With permission of OUP.
• Muscles within the shoulder girdle:
• Move the arm and control movements at the shoulder joint
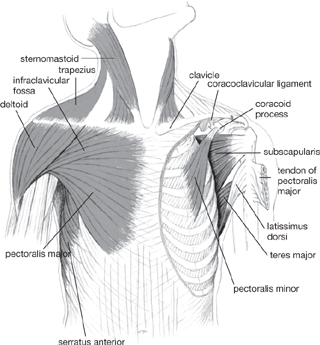
Fig. 5.15 Muscles of the axilla and shoulder (anterior view).
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p62 (Oxford, 2005). With permission of OUP.
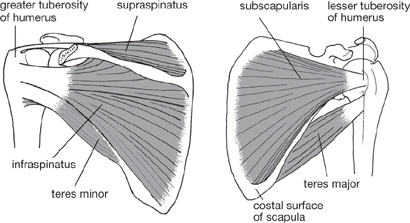
Fig. 5.16 Supraspinatus, infraspinatus, teres minor; acromion removed (posterior view).
Subscapularis and teres major (anterior view).
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p62 (Oxford, 2005). With permission of OUP.
• Muscles in the arm in the anterior compartment (Fig. 5.17):
• Muscles in the arm in the posterior compartment:
• Muscles in the forearm in the anterior compartment (Fig. 5.18):
 Flexor digitorum superficialis and profundus.
Flexor digitorum superficialis and profundus.
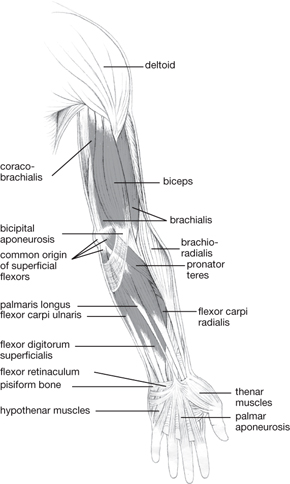
Fig. 5.17 Superficial flexor muscles of arm and forearm.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p81 (Oxford, 2005). With permission of OUP.
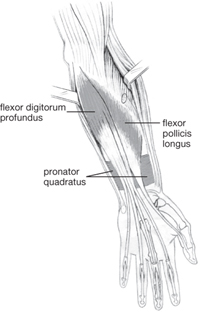
Fig. 5.18 Deep flexor muscles of the forearm.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p81 (Oxford, 2005). With permission of OUP.
• Muscles in the forearm in the posterior compartment (Figs 5.19, 5.20):
 Extensor digitorum, indicis, and digiti minimi
Extensor digitorum, indicis, and digiti minimi
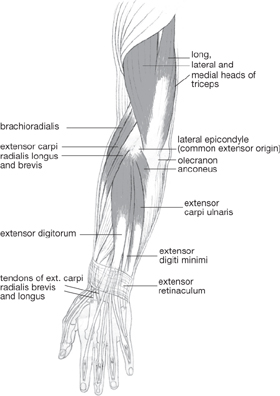
Fig. 5.19 Superficial extensor muscles of arm and forearm.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p83 (Oxford, 2005). With permission of OUP.
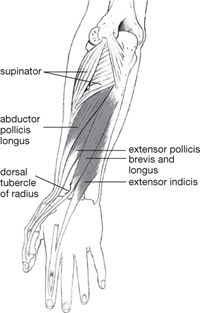
Fig. 5.20 Deep extensor muscles of forearm.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p83 (Oxford, 2005). With permission of OUP.
• Muscles of the hand (Fig. 5.21):
• Move the thumb, little finger
 Thenar and hypothenar eminences
Thenar and hypothenar eminences
• Move fingers from side to side
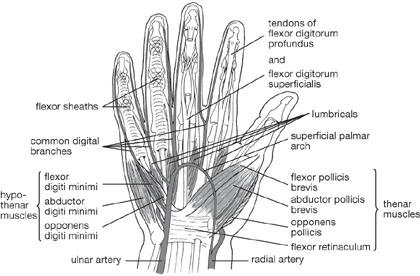
Fig. 5.21 Superficial aspect of palm.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p91 (Oxford, 2005). With permission of OUP.
Motor and sensory fibres are distributed to particular nerves that supply muscles groups, joints, and skin via the brachial plexus (Figs 5.22, 5.23). Spinal nerve root supply is indicated by superscript.
Roots arise from the anterior primary rami of cervical spinal nerves C5–C8 in the neck and thoracic nerve T1 in the thorax. The spinal nerves are formed from the unification of ventral (motor) and dorsal (sensory) nerve roots from the spinal cord.
• The long thoracic nerve arises from C5, 6, and 7
• The dorsal scapular nerve arises from C5.
Trunks are formed in the posterior triangle of the neck. C5 and C6 unite to form the upper, C7 becomes the middle, C8 and T1 unite to form the lower. Trunks pass down and laterally over the first rib.
• The suprascapular nerveC5,6 and the nerve to subclaviusC5,6 arise from the upper trunk.
Beneath the clavicle, fibres from each trunk redistribute into anterior and posterior divisions. Anterior supply flexor compartments and the overlying skin, posterior supply extensor equivalents.
Divisions recombine to form three cords: lateral, medial, and posterior to the axillary artery.
• The lateral pectoral nerveC5,6,7 arises from the lateral cord
• The medial pectoral nerveC8, T1 and the medial cutaneous nervesC8, T1 of arm and forearm arise from the medial cord
• The upper subscapular nerveC5,6, thoracodorsal nerveC6,7,8, and lower subscapular nerveC5,6 arise from the posterior cord.
Terminal nerves arise from the cords.
• The lateral cord gives the musculocutaneous nerveC5,6,7 and contributes to the median nerveC5,6,7,8 T1
• The medial cord gives the ulnar nerveC8, T1 and contributes to the median nerve
• The posterior cord gives the axillary nerveC5,6 and the radial nerveC5,6,7,8 T1.
Flexor (anterior) compartments are supplied by nerves originating from the lateral and medial cords.
• The musculocutaneous nerve (Fig. 5.24) supplies coracobrachialis, biceps, brachialis. It then continues as the lateral cutaneous nerve of the forearm, which supplies skin of the lateral forearm
• Median nerve branches (Fig. 5.25) supply:
• Flexor muscles (except flexor carpi ulnaris and medial half of flexor carpi profundus), thenar eminence, lumbricals
• Skin of the palm; skin of palmar surface and nail bed of lateral 3½ digits
• Ulnar nerve branches (Fig. 5.26) supply:
• Flexor carpi ulnaris and medial half of flexor carpi profundus, muscles of the hand except thenar eminence, lumbricals
• Skin of palmar and dorsal aspects of medial 1½ digits.
Fig. 5.22 Branchial plexus: schematic diagram of roots, trunks, cords, and branches.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p112 (Oxford, 2005). With permission of OUP.
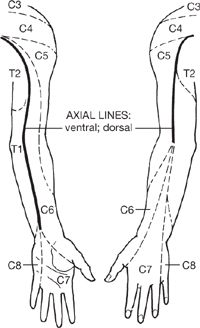
Fig. 5.23 Dermatomes of upper limb: note the axial lines.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p114 (Oxford, 2005). With permission of OUP.
• Extensor (posterior) compartments are supplied by nerves originating from the posterior cord (Fig. 5.27)
• Axillary nerve branches supply:
• Teres major and minor and deltoid
• The badge of skin overlying the deltoid
• Radial nerve branches supply:
• Skin of the posterior aspect of the upper limb (as the posterior cutaneous nerves of the arm and forearm)
• The dorsal aspect of the lateral 3½ digits.
Tendon reflexes (OHCM6 pp.55, 330, 331) are fundamental to the examination of the peripheral nervous system. Diminished or brisk reflexes suggests lesion of the upper or lower motor neurone (upper motor neurones are first-order neurones which do not leave the central nervous system; lower motor neurones are the second-order neurones—the cranial and spinal nerves).
By tapping specific tendons, a monosynaptic reflex arc is triggered. The muscle spindle is stretched, which stimulates afferent fibres, and these synapse with efferent motor neurones of the anterior horn. This results in the muscle contracting and a subsequent ‘jerk’.
Important ‘jerk’ reflexes in the upper limb and their nerve roots are:
Fig. 5.24 Musculocutaneous nerve: supply to muscles.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p116 (Oxford, 2005). With permission of OUP.
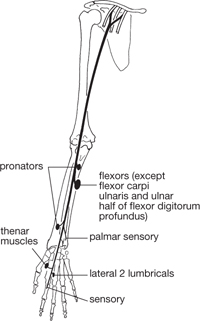
Fig. 5.25 Median nerve: supply to muscles.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p116 (Oxford, 2005). With permission of OUP.
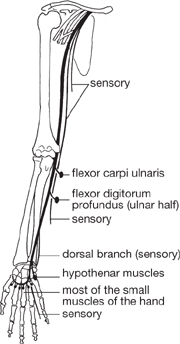
Fig. 5.26 Ulnar nerve: supply to muscles.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p117 (Oxford, 2005). With permission of OUP.
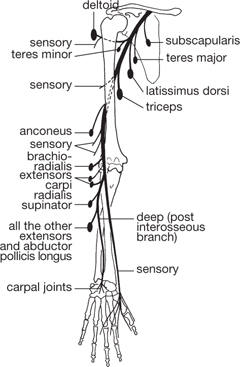
Fig. 5.27 Posterior cord, axillary and radial nerves: supply to muscles.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p120 (Oxford, 2005). With permission of OUP.
The upper limb is supplied by the subclavian artery which arises on the left from the aorta and on the right from the brachiocephalic trunk. The subclavian artery passes beneath the clavicle and enters the axilla, giving branches to the anterior and lateral chest wall.
At the outer border of the first rib, it becomes the axillary artery and the artery accompanies the brachial plexus, located medially within the axillary sheath.
Branches:
• To the chest wall and breast (superior and lateral thoracic arteries)
• To medial superficial shoulder tissue (thoracoacromial artery)
• Around the upper shaft of the humerus (circumflex humeral artery)
• Along the lateral scapula (subscapular artery).
On leaving the axilla, the artery becomes the brachial artery. It runs along the medial aspect of the arm; its superficial lie allows it to be felt at the front of the elbow.
Branches:
• Near its origin to supply posterior compartment muscles and elbow joint (profunda brachii artery); this follows the course of the radial nerve
• To supply the humerus (nutrient artery) and anterior compartment muscles.
As the artery enters the forearm, it divides into the radial artery and the ulnar artery, which pass towards the wrist beneath the superficial muscles in the anterior compartment.
The ulnar artery branches soon after formation to establish the common interosseous artery, which in turn branches into the anterior (to the flexor compartment) and the posterior (to the extensor compartment) interosseous arteries.
The ulnar artery and radial arteries pass through the wrist into the palm and divide into:
• Superficial branches which anastomose to form the superficial palmar arch
• Deep branches which anastomose to form the deep palmar arch.
The superficial arch gives rise to four digital arteries; the deep arch gives rise to three metacarpal arteries. These unite to supply the digits. Princeps pollicis and radialis indicis arise from the radial artery to supply the thumb and index finger.
The radial pulse can be felt at the wrist where the artery lies on the distal radius.
In general, muscles and joints are supplied by adjacent arteries. Anastomoses between adjacent arteries are present at joints and provide a collateral circulation to sustain perfusion should the primary supply be compromised by joint movement.
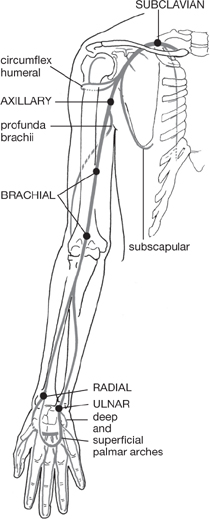
Fig. 5.28 Major arteries of the upper limb: pressure points for arrest of haemorrhage.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p102 (Oxford, 2005). With permission of OUP.
Venous drainage can be divided into superficial and deep systems.
Digital veins drain along with veins in the palm into the dorsal venous arch on the back of the hand. This network is drained by superficial veins:
• The ulnar side of the arch drains to the basilic vein, which ascends along the medial forearm
• The radial side is drained by the cephalic vein, which passes laterally up the forearm.
Tributaries draining superficial tissues join these two vessels as they ascend.
The two veins are connected by the median cubital vein which crosses the front of the elbow in the cubital fossa, and is often used for venepuncture.
Deep veins (the venae comitantes) usually run in pairs alongside arteries. Above the elbow, the basilic vein unites with veins draining deeper structures of the forearm and upper arm (the venae comitantes of the brachial artery). The united vessels form the axillary vein, into which other venae comitantes in turn drain. The cephalic vein drains into the axillary vein beneath the clavicle.
The axillary veins progress into the base of the neck where they become the subclavian veins. These unite with veins draining the head to form the superior vena cava.
Lymphatic drainage parallels venous drainage.
There are superficial and deep lymphatic vessels, with few interconnections. Superficial drainage:
• Of the radial side is through vessels accompanying the cephalic vein
• Of the ulnar side occurs through vessels running alongside the basilic vein.
Deep tissue drains through vessels accompanying the deep blood vessels.
Most superficial and deep vessels ultimately drain into the axillary lymph nodes which lie along the axillary artery. There are up to 50 such nodes:
• The lateral nodes, medial to the axillary vein, drain most of the lymph from the arm
• In turn, the lateral nodes drain into the central nodes
• The central nodes feed into the apical nodes.
Vessels accompanying the cephalic vein drain directly into the apical nodes.
Lymph passes from the nodes to the subclavian lymph trunk alongside the subclavian artery. The trunk joins others, including the thoracic duct on the left side, to drain into the venous system at the unification of the subclavian and internal jugular veins.
Fig. 5.29 Superficial veins of upper limb: position of groups of lymph nodes.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p102 (Oxford, 2005). With permission of OUP.
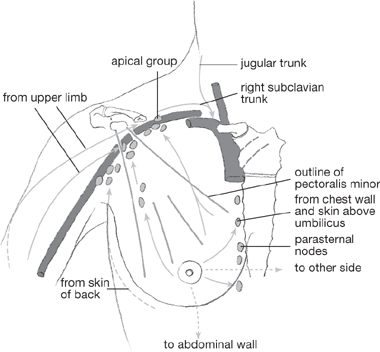
Fig. 5.30 Lymph nodes of the axilla and the internal thoracic chain.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p105 (Oxford, 2005). With permission of OUP.
The axilla:
• Lies between the upper end of the arm and the chest wall
• Is continuous above with the space between the upper ribs and the shoulder girdle
• Inferior limit is the armpit
• Anterior wall is formed by pectoralis major and minor, together with the clavicle
• Medial wall is formed by the upper ribs and serratus anterior
• Posterior wall is formed by the scapula and muscles covering its anterior surface.
The axilla contains:
• The cords and branches of the brachial plexus
which are surrounded and protected by fat.
The cubital fossa:
• Is a triangular region anterior to the elbow joint
• Lateral boundary is brachioradialis
• Medial boundary is pronator teres
• Base is the line between the epicondyles of the humerus
The biceps tendon can be palpated within the cubital fossa. The brachial artery and median nerve are found medial to the tendon within the fossa. The radial and ulnar nerves are outside the fossa.
The carpal tunnel (Fig. 5.31) is formed by the concavity of the palmar surface of the carpal bones and its overlying flexor retinaculum, a fibrous band attached to the pisiform, hook of hamate, scaphoid, and trapezium. The tunnel contains:
• The long flexor tendons of the thumb and fingers (except that of flexor carpi radialis)
but lacks veins and arteries.
Compression of the median nerve results in carpal tunnel syndrome (OHCM8 p.507), with motor and sensory impairment.
The anatomical snuffbox is a depression on the dorsal aspect of the hand. It is defined by:
• The scaphoid and trapezium, which form its base
• The tendons of abductor pollicis longus and extensor pollicis brevis on the anterior aspect
• The tendon of extensor pollicis longus posteriorly.
The radial artery passes through the snuffbox. Scaphoid fractures result in acute tenderness in this region.
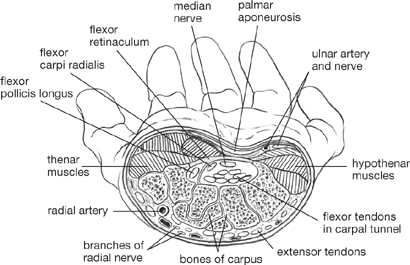
Fig. 5.31 Carpal tunnel and contents (tendon sheaths not shown); transverse section.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p93 (Oxford, 2005). With permission of OUP.
The pelvic girdle (Fig. 5.32) is a ring of bones which surrounds the caudal body cavity and comprises two hip bones (or innominate bones) and the sacrum. Together, these bones transmit the weight of the structures above to the lower limbs and protect and support the pelvic organs.
• Are joined at the anterior aspect by a cartilaginous joint—the pubic symphysis
• Are formed from three separate bones:
• The ileum, a flat blade which is superior to
• The pubis, an arch of bone, which is anterior to
• The ischium, which forms the bony prominence of the buttock
• Articulate with the femur at a socket (the horseshoe-shaped acetabulum), which is the site at which the three constituent bones are fused
• Articulate with the sacrum at sacro-iliac joints.
• Comprises five fused vertebrae
• At its superior aspect with the 5th lumbar vertebra
• Inferiorly with the coccyx, formed from three to five rudimentary fused vertebrae
• Laterally with the ileum on each side.
The bones of the legs comprise the thigh bone—the femur; the knee cap—the patella; the shin bone—the tibia; the fibula.
Fig. 5.32 Anterior aspect of adult (female) pelvis.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p129 (Oxford, 2005). With permission of OUP.
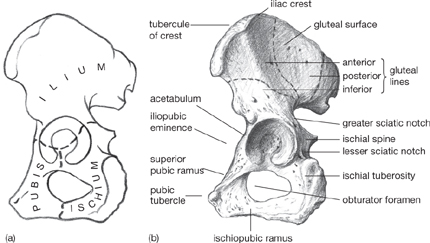
Fig. 5.33 (a) Diagram of pelvis (lateral view) showing fusion lines where the three constituent bones (ilium, ischium, pubis) meet. (b) Lateral aspect of adult pelvis.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p130 (Oxford, 2005). With permission of OUP.
• Is the longest bone in the body
• Possesses a smooth, rounded head, which articulates with the acetabulum and permits movement in any direction
• Has a prominent neck which makes an angle of 125° with the shaft
• Slopes in a medial direction as it descends, making an angle of 170° with the shaft of the tibia
• Distal end is flared, with the lateral (larger) and medial condyles, which articulate with the tibia
• Is often fractured at the neck.
• Is a roughly circular sesamoid bone in the tendon of quadriceps
• Is located anterior to the knee joint
• Posterior surface articulates with the condyles of the femur, with the lateral condyle providing a stop to resist lateral dislocation
• Glides in the groove between the condyles, and so acts as a pulley to improve leverage.
• Transfers weight from the femur to the talus
• Possesses a flattened plateau with lateral and medial condyles which articulate with those of the femur
• Shaft is straight, triangular in cross-section and tapered towards its distal end
• The anterior border and medial surface of the shaft lie subcutaneously and constitute a common site for open fractures
• Articulates with the superior bones of the talus
• Projects inferiorly as the medial malleolus, which articulates with the medial talus forming one half of the mortice to stabilize the ankle joint
• Derives its name from the similarity of its shape to a Roman flute.
• Is a long, thin (‘brooch’) bone, with head, neck, shaft, and inferior end
• Is not part of the knee joint
• Provides a framework for muscle attachments, protects blood vessels, participates in the ankle joint
• Head articulates with the lateral condyle of the tibia
• At its inferior end articulates with the fibular notch on the lateral aspect of the inferior tibia
• At its most inferior, constitutes the lateral malleolus, the other half of the mortice.
Fig. 5.34 Bones of the lower limb and pelvic girdle: anterior view.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p130 (Oxford, 2005). With permission of OUP.
The bones of the foot comprise the seven bones of the main part of the foot—the tarsus—together with the five bones of the forefoot—the metatarsals—and 14 bones of the toes—the phalanges.
The tarsus bones (Fig. 5.35), located distal to the ankle joint, comprise the:
• Body articulates superiorly with the tibia and, to the sides, with the lateral malleolus and medial malleolus
• Possesses a neck connecting the body to a head
• Head is rounded for articulation distally with the navicular bone
• Makes three small articulations inferiorly with the calcaneus bone.
• Articulates with the talus bone superiorly
• Makes an articulation at its anterior surface with the cuboid bone
• Receives the insertion of the tendocalcaneus (Achilles’ tendon) of superficial flexor muscles on its posterior aspect
• Has two pronounced tubercles on its undersurface.
• Articulate at their posterior aspect with the navicular bone
• Articulate anteriorly with the first three metatarsals
• Are wedge-shaped so that together they help to maintain a transverse arch.
• Articulates with the fourth and fifth metatarsals.
• Are equivalent to the metacarpals of the hand
• Comprise a base, shaft, and head
• Articulate anteriorly with the first row of phalanges.
The first metatarsal is not as free-moving as the first metacarpal. The second metatarsal forms a mortice joint between the lateral and medial cuneiforms to limit its movements. The heads of the metatarsals, together with the tubercles of the calcaneus form the longitudinal arch through which the weight of the body is distributed.
• Are shorter and thicker than those in the hand
• Possess a base, shaft, and head
• Are three in number, except in the great toe, where there are only two.
Fig. 5.35 Tarsal bones: dorsal view.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p132 (Oxford, 2005). With permission of OUP.
• Midline fibrocartilaginous joint between the two pubic bones
• Superior pubic ligament above
• Arcuate ligament spanning the pubic arch
• Movements are usually limited, but mobility increases during pregnancy.
• Synovial joints between the anterior surface of the sacrum and articular surface of the ileum (of the innominate bone)
• Irregular surfaces within the joint interlock
• Joint is strengthened by posterior, anterior, and interosseous sacroiliac ligaments
• Sacrotuberous ligaments (between lateral sacrum, coccyx, and ischial tuberosity) and sacrospinous ligaments (between lateral sacrum, coccyx, and ischial spine) resist forward rotatory thrust from weight of spine on sacrum.
• Ball-and-socket joint, capable of movements in any plane
• Between head of femur and cartilage lining the horseshoe outline of the acetabulum
• For stability, the socket is far deeper than the equivalent in the shoulder joint
• Possesses a stabilizing ring of fibrocartilage (the labrum) around the margin
• The transverse ligament bridges the notch of the acetabulum to complete the socket
• Round ligamentum teres runs from the transverse ligament to fovea at centre of head of femur
• Capsule lined by synovial membrane and strengthened by:
• Anterior Y-shaped iliofemoral ligament
Fig. 5.36 Pelvis showing sacrotuberous and sacrospinous ligaments (and also inguinal ligament).
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p140 (Oxford, 2005). With permission of OUP.
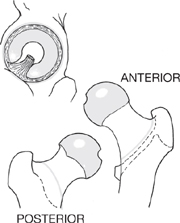
Fig. 5.37 Attachments of capsule of hip joint.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p140 (Oxford, 2005). With permission of OUP.
• Compound hinge synovial joint with hyaline cartilage
• Primary movements are flexion and extension; some rotation possible
• Between medial, lateral condyles of femur and tibial plateau, posterior patella
• Femoral and tibial articulating surfaces are partially replaced by two crescent-shaped fibrocartilaginous menisci
• Encapsulated, with patella contributing the anterior portion
• Patellar retinacula (fascial expansions of tendons) confer further support
• Medial (tibial) and lateral (fibular) collateral ligaments strengthen the capsule
• Posterior (oblique popliteal) ligament resists torsional stresses
• Anterior and posterior cruciate ligaments lie outside the capsule; these keep the articulating surfaces apposed
• Synovial membrane extends superiorly to form suprapatellar bursa, which facilitates movements of quadriceps over femur
• Prepatellar bursa lies in front of the patella; subcutaneous and deep infrapatellar bursae sandwich the patellar tendon (termination of quadriceps).
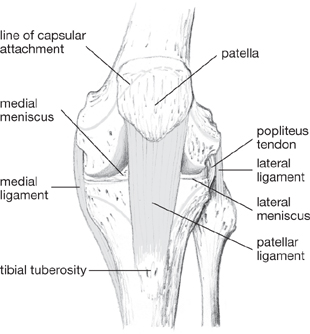
Fig. 5.38 Knee joint: anterior view showing capsule attachments and ligaments.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p150 (Oxford, 2005). With permission of OUP.
Fig. 5.39 Cruciate ligaments, anterior view.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p151 (Oxford, 2005). With permission of OUP.
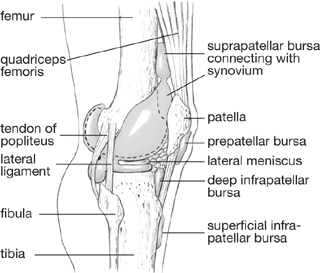
Fig. 5.40 Synovial membrane and bursae of knee.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p152 (Oxford, 2005). With permission of OUP.
• Superior plane synovial joint between head of fibula and lateral condyle of tibia
• Inferior fibrous joint between lower end of fibula and tibia
• Shafts united by interosseous membrane, which provides a framework for muscle attachments.
• Synovial hinge joint, permitting flexion and extension
• Between upper surface of talus and lower ends and malleoli of tibia and fibula
• Malleoli restrict abduction and adduction
• Anterior flaring of talus forms wedge shape; in dorsiflexion the wedge is driven between the malleoli to maximize stability
• Encapsulated, with reinforcing medial (deltoid) and lateral (anterior talofibular, calcaneofibular, posterior talofibular) ligaments
• Lateral ligament is weaker than the medial one—most commonly damaged in a sprain
• Extensor retinacula retain extensor tendons to dorsum of foot
• Superficial between anterior borders of lower tibia and fibula
• inferior Y-shaped between calcaneus and medial malleolus, plantar fascia
• Flexor retinaculum retains flexor tendons
• Runs from medial malleolus to calcaneus and plantar fascia
• The protective plantar aponeurosis extends from calcaneus to the flexor sheaths at the base of the toes.
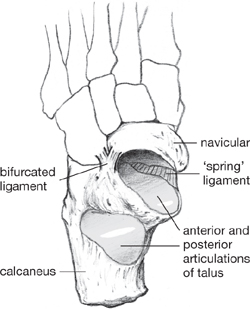
• A compound joint comprising:
• A posterior synovial plane joint (the talocalcaneal joint) strengthened by the intraosseous ligament
• An anterior synovial ball-and-socket joint (the talocalcaneonavicular joint) strengthened by the calcaneonavicular (‘spring’) ligament
• The curvatures of the two articulating portions of the talus permit inversion and eversion.
• A compound joint comprising:
• Calcaneocuboid joint (a synovial joint) strengthened by the bifurcated ligament
• The talonavicular articulation of the talocalcaneonavicular joint
• These also permit a degree of inversion and eversion
• Other tarsal joints—between the three cuneiform bones; cuneiform bones and the navicular bone; lateral cuneiform and cuboid bones; cuboid and navicular bones—are strengthened by interosseous, plantar and dorsal ligaments. These joints permit very little movement
• Tarsometatarsal joints—synovial plane
• Intermetatarsal joints—synovial plane
• Metatarsophalangeal joints—synovial condylar
• Interphalangeal joints—synovial hinge.
Fig. 5.41 Anterior attachments of capsule of left ankle joint, and inferior tibio-fibular joint.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p162 (Oxford, 2005). With permission of OUP.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p171 (Oxford, 2005). With permission of OUP.
Nerve supply is indicated by superscript.
• Psoas majorlumbar nerves L1–4
• Gluteus maximusinferior gluteal nerve
• The hamstring musclessciatic nerve
• Gluteus medius and minimussuperior gluteal nerve
• Tensor fasciae lataesuperior gluteal nerve
• Adductor longusobturator nerve
• Adductor magnusobturator nerve
• Adductor brevisobturator nerve
• Piriformissacral nerves S1–2
• Obturator internusnerve to obturator internus
• Quadratus femorisnerve to quadratus femoris.
• Peroneus longus and brevisdeep peroneal nerve
• Tibialis anteriordeep peroneal nerve
• Extensor hallucis longusdeep peroneal nerve
• Flexor hallucis longustibial nerve and brevismedial plantar nerve
• Flexor digitorum longustibial nerve and brevismedial plantar nerve
• Flexor digiti minimi brevismedial plantar nerve
• Flexor accessoriusmedial plantar nerve
• Extensor hallucis longusdeep peroneal nerve
• Extensor digitorum longus and brevisdeep peroneal nerve
• Lateral rotation (‘unlocking’)
• Sitting cross-legged (the ‘tailor’s position’)
• Dorsiflexion (foot points up)
• Plantar flexion (foot points down)
• Muscles of the buttocks (gluteal region):
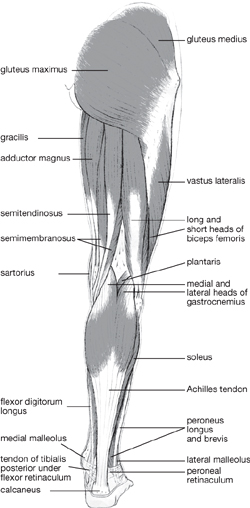
Fig. 5.43 Muscles of the back of the lower limb.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p154 (Oxford, 2005). With permission of OUP.
• Muscles of the thigh in the anterior compartment:
• Flex and rotate the hip; extend and flex the knee
• Muscles of the thigh in the posterior compartment:
• Flex the knee; extend the hip
• Muscles of the thigh in the medial (adductor) group:
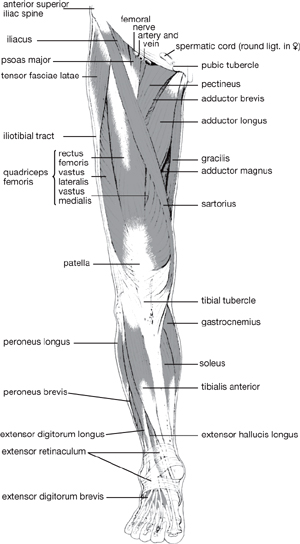
Fig. 5.44 Muscles of the front of the lower limb.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p155 (Oxford, 2005). With permission of OUP.
• Muscles of the lower leg in the anterior compartment:
• Extend the toes; dorsiflex, invert the foot
• Muscles of the lower leg in the posterior compartment:
• Flex the toes; plantar flex the foot
• Muscles of the lower leg in the lateral compartment:
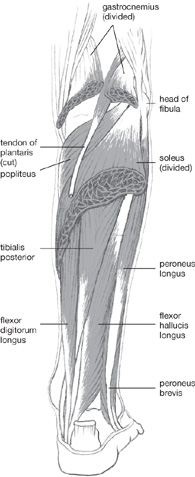
Fig. 5.45 Deep muscles of the calf.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p164 (Oxford, 2005). With permission of OUP.
• Move the toes from side to side
 Abductor and adductor hallucis
Abductor and adductor hallucis
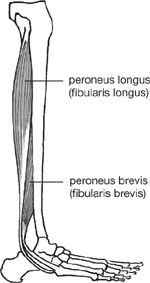
Fig. 5.46 Peroneus longus, peroneus brevis.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p171 (Oxford, 2005). With permission of OUP.
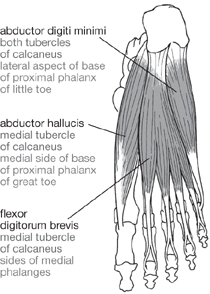
Fig. 5.47 Sole of foot, muscle layer 1.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p172 (Oxford, 2005). With permission of OUP.
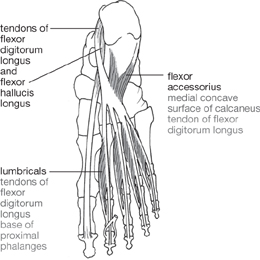
Fig. 5.48 Sole of foot, muscle layer 2.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p172 (Oxford, 2005). With permission of OUP.
Spinal nerve root supply indicated by superscript.
A similar arrangement to that in the upper limb applies. Nerve supplies originate from the lumbosacral plexus which comprises:
• A lumbar part, formed from lumbar spinal nerve roots L2–5 located within psoas major
• A sacral part, formed from sacral spinal nerve roots S1–3 lying on the posterior pelvic wall.
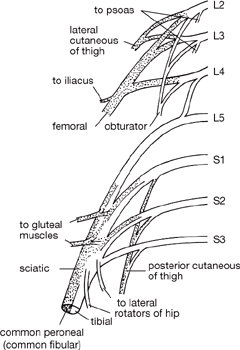
Lumbar spinal nerve roots provide nerves to psoas majorL1,2,3,4, the ilioinguinal nerveL1, the genitofemoral nerveL1,2, and the lateral cutaneous nerve of the thighL2,3, and give rise to two major branches:
• Posterior divisions are arranged as the femoral nerveL2,3,4 which:
• Emerges from the lateral side of psoas major
• Passes under the inguinal ligament
• Gives off the intermediate and medial cutaneous nerves of the thigh to supply overlying skin and the saphenous nerve, which supplies medial aspects of knee and lower leg
• Provides terminal branches supplying anterior (extensor) muscles
• Anterior divisions are arranged as the obturator nerveL2,3,4 which:
• Emerges from the medial side of psoas major at pelvic brim
• Passes through obturator foramen of innominate bone
• Gives off a nerve to obturator externusL3,4
• Enters the adductor compartment and supplies:
A branch of lumbar spinal nerve L4 unites with spinal nerve L5 to form the lumbosacral trunk. This combines with sacral spinal nerves S1–3 to form the sciatic nerve.
Superior to the input from S3, the superiorL4,5,S1,2 and inferior gluteal nervesL5,S1,2 arise to supply the gluteal muscles and tensor fascia latae. Other branches include the nerve to quadratus femorisL4,5,S1, the nerve to obturator internus L5, S1,2, the posterior cutaneous nerve to the thighS1,2,3, and the pudendal nerveS2,3,4.
The sciatic nerve:
• Descends medial to psoas major, over the sacroiliac joint, then through the greater sciatic foramen, under gluteus maximus into the posterior compartment
• Gives branches to semimembranosus, semitendinosus, biceps femoris, adductor magnus.
Fig. 5.49 Dermatomes of lower limb; note the axial lines.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p188 (Oxford, 2005). With permission of OUP.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p188 (Oxford, 2005). With permission of OUP.
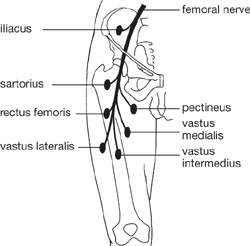
Fig. 5.51 Femoral nerve; supply to muscles.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p189 (Oxford, 2005). With permission of OUP.
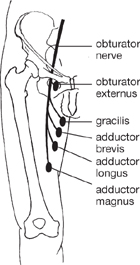
Fig. 5.52 Obturator nerve; supply to muscles.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p189 (Oxford, 2005). With permission of OUP.
• Divides at the mid-length of the thigh into:
• The tibial nerveL4,5,S1,2,3 which:
 Provides branches to flexor muscles of the leg, muscles of sole of foot
Provides branches to flexor muscles of the leg, muscles of sole of foot
 Gives rise to the medial and lateral plantar nerves; contributes to the sural nerve and calcaneal nerve
Gives rise to the medial and lateral plantar nerves; contributes to the sural nerve and calcaneal nerve
 Supplies skin of calf, heel, and sole through these sensory nerves
Supplies skin of calf, heel, and sole through these sensory nerves
• The common peroneal nerveL4,5,S1,2 which:
 Provides branches to extensor muscles of leg and foot—the peroneal muscles
Provides branches to extensor muscles of leg and foot—the peroneal muscles
 Gives rise to the superficial and deep peroneal nerves; contributes to the sural nerve and calcaneal nerve
Gives rise to the superficial and deep peroneal nerves; contributes to the sural nerve and calcaneal nerve
 Supplies skin on lateral aspect of leg and dorsal surface of foot.
Supplies skin on lateral aspect of leg and dorsal surface of foot.
Tendon reflexes (OHCM6 pp.55, 330, 331) are fundamental to the examination of the PNS. Diminished or brisk reflexes suggest lesion of the lower or upper motor neurone.
Important ‘jerk’ reflexes in the lower limb and their nerve roots are:
• Knee jerk of patellar tendon: L3, L4
• Ankle jerk of Achilles tendon: L5, S1.
In addition, a plantar reflex can be elicited. On stroking the sole of the foot (in a specific manner), the toes normally point downwards (plantar flex). If the toes point upwards (dorsiflex) and spread outwards, this is a positive test result (or Babinski response) and indicates an upper motor neurone lesion.
Fig. 5.53 Common peroneal nerve: supply to muscles.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p192 (Oxford, 2005). With permission of OUP.
Fig. 5.54 Gluteal, sciatic, and tibial nerves.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p190 (Oxford, 2005). With permission of OUP.
Fig. 5.55 Sciatic and tibial nerves: supply to muscles.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p191 (Oxford, 2005). With permission of OUP.
The lower limb is supplied by the external iliac artery. The superior gluteal and inferior gluteal artery which arise from the internal iliac artery pass either side of piriformis to supply the gluteal region.
The external iliac artery passes under the inguinal ligament at its midpoint and enters the thigh.
At this point, it lies in the femoral triangle, and becomes the femoral artery which lies alongside the femoral vein within the femoral sheath.
The deep femoral artery:
• Arises from the femoral artery and runs between adductors longus and magnus
• Provides circumflex arteries which anastomose with descending branches of the gluteal arteries around the upper femur (trochanteric and cruciate anastomoses) and perforating arteries which supply muscles of the thigh.
The (superficial) femoral artery then passes under sartorius, runs medially down the thigh, passes between the adductor and hamstring components of adductor magnus, and enters the popliteal fossa.
From this point, the artery becomes the popliteal artery that provides genicular branches which anastomose around the knee joint. It exits the fossa and divides into anterior and posterior tibial arteries.
The anterior tibial artery:
• Runs over the upper border and then descends in front of the interosseous membrane as far as the front of the ankle joint, with branches supplying anterior compartment (extensor) muscles of the lower leg
• Then becomes the dorsalis pedis artery which runs over the dorsal aspect of the foot and supplies the toes through:
• Dorsal first metacarpal and arcuate branches
• A branch which anastomoses with the deep plantar arch in the sole.
The posterior tibial artery:
• Descends the posterior (flexor) compartment
• Gives rise to the peroneal artery which supplies the lateral compartment of the leg
• Passes behind the medial malleolus, after which it divides into medial and lateral plantar arteries under the flexor retinaculum
• The lateral plantar artery is larger and runs to the lateral aspect of the sole; its deep branch forms the deep plantar arch from which plantar metacarpal branches supply the toes
• The medial plantar artery runs on the medial aspect of the sole; branches join plantar metacarpal branches from the lateral artery.
Fig. 5.56 Major arteries of lower limb.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p178 (Oxford, 2005). With permission of OUP.
A similar arrangement exists to that in the upper limb. Drainage can be divided into superficial and deep systems, connected by communicating veins.
The superficial system drains skin and superficial tissue. Veins from the toes pass in a dorsal direction to the dorsal venous arch which drains:
• Medially to the small saphenous vein which passes behind the lateral malleolus, over the back of the calf, and drains into the popliteal vein
• Laterally to the great saphenous vein which passes in front of the medial malleolus, along the medial aspect of the calf and thigh, enters the femoral triangle, and drains into the femoral vein.
The deep system comprises the venae comitantes accompanying the tibial arteries, which become, first, the popliteal vein and, subsequently, the femoral vein. The deep veins in the posterior compartment of the calf:
• Form an extensive network—the soleal plexus
• Are connected by perforating veins at multiple levels to the great saphenous vein
• Are emptied by the contraction of surrounding muscles which force blood upwards—the ‘muscle pump’.
Veins in the lower limb have many valves to minimize hydrostatic pressure associated with upright posture and thereby facilitate venous return.
A similar pattern exists to that in the upper limb. Superficial lymphatic vessels draining skin and subcutaneous structures accompany superficial veins; deep tissue drains though deep lymphatic vessels which run with deep blood vessels.
Lymph nodes in the groin are arranged in superficial and deep groups. Superficial nodes are arranged as:
• A longitudinal chain along the great saphenous vein
• A horizontal chain along the line of the inguinal ligament
which drain the superficial tissues of the lower limb and the trunk, below the umbilicus.
Deep nodes receive the drainage from the superficial nodes. They are located medial to the femoral vein in the femoral canal and drain deeper tissues.
Lymphatic vessels leave the deep nodes and convey lymph to nodes along the external iliac artery, which in turn drain into paraaortic nodes. Lymph passes through the cisterna chyli and thoracic duct, and is returned to the circulation at the unification of the subclavian and internal jugular veins.
Fig. 5.57 Major veins, lymphatic channels (arrows), and lymph nodes of the lower limb.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p182 (Oxford, 2005). With permission of OUP.
The femoral triangle boundaries are:
• Lateral—the medial border of sartorius
• Medial—the medial border of adductor longus.
The floor is contributed by:
The roof is defined by fascia and is punctured by the saphenous opening.
The triangle contains:
• The femoral sheath enveloping the femoral artery and vein and the femoral canal (containing lymphatic vessels)
The femoral vessels and branches of the femoral nerve pass through the adductor canal—a channel which starts at the apex of the triangle and runs beneath sartorius towards the medial aspect of the thigh. It is defined by:
• Adductor longus and, inferiorly, adductor magnus (posterior wall)
• Vastus medialis (lateral wall)
• Fascia-enveloping sartorius (roof).
The femoral artery and vein pass into the popliteal region through an opening in adductor magnus (the adductor hiatus).
The diamond-shaped popliteal fossa boundaries are:
• Superior—biceps femoris (lateral), semitendinosus and semimembranosus (medial)
• Floor—posterior surface of lower femur, oblique popliteal ligament, posterior surface of tibia, popliteus
The fossa contains:
• Popliteal artery (the continuation of the femoral artery)
The vertebral column is the main bony supporting structure of the trunk and is critical for locomotion, support of the upper trunk and head, stabilization of the pelvis, posture, and protection of the delicate structures of the spinal cord. It consists of seven cervical vertebrae, 12 thoracic vertebrae, five lumbar vertebrae, five fused sacral vertebrae forming the sacrum, and three to five fused coccygeal vertebrae forming the coccyx. In between the cervical, thoracic, and lumbar vertebrae, the intervertebral discs separate the bony elements (Figs 5.58, 5.59).
In utero, the spinal column develops with a single mild curvature in the median plane which is convex when viewed from a posterior position. During infancy, extra curvatures develop. Four curvatures are apparent in the adult. When viewed from a posterior angle, cervical and lumbar curvatures are convex, while thoracic and sacral curvatures are concave. Excessive curvature of the spine can result in disability. Kyphosis (OHCM6 p.66), which follows erosion of the anterior areas of the vertebral bodies, is an increase in the thoracic curvature, while lordosis is an increase in the lumbar curvature (this occurs naturally during pregnancy to accommodate the fetus). Scoliosis (OHCM6 p.66) is an abnormal curvature of the spine in the coronal plane. It can result from leg length discrepancies, unilateral weakness of spinal muscles, or vertebral abnormalities.
Vertebrae from different parts of the spinal column share certain key features. The vertebral body is the most anterior part of a vertebra and is critical for weight-bearing and support. From the posterior aspect of each vertebral body arises a vertebral arch which completely encloses the vertebral foramen containing the spinal cord. The arch comprises two pedicles—short processes arising from either side of the vertebral body, connected by a single lamina. On either side of the vertebral arch there is a bony spinous projection (transverse process) and a spinous process arises from the peak of the two laminae. It projects inferiorly and overlaps the vertebral bone below. Superior and inferior articular processes are found at each join between the laminae and pedicles and these articulate with the corresponding processes on the vertebral bodies immediately above and below.
• The first two cervical vertebrae are important in attaching the skull to the vertebral column (atlanto-occipital joint) and are atypical
• The atlas (C1) has no body and is a ring-like structure which articulates with the skull permitting nodding motions of the head
• The axis (C2) includes a peg (odontoid peg or dens) which sits in the ring of the atlas. The odontoid peg allows rotation of the head and is formed by the fusion of the body of C1 with C2 during development
• Alar ligaments run from the lateral sides of the foramen magnum to the side of the odontoid process, preventing excessive rotation of the head.
Fig. 5.58 Midline sagittal section through lumbar spine to show discs and ligaments.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p204 (Oxford, 2005). With permission of OUP.
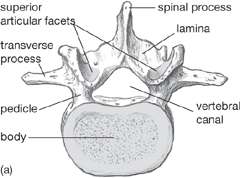
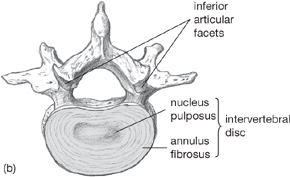
Fig. 5.59 Lumbar vertebrae viewed (a) from above, (b) from below; intervertebral disc.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p205 (Oxford, 2005). With permission of OUP.
• The transverse ligament of the atlas extends between the lateral mass tubercles of C1, forming a sling around the odontoid process
• The cruciform ligament is a cross-shaped ligament between the occipital bone above and the body of C2 below
• The tectorial membrane is a continuation of the posterior longitudinal ligament, covering the alar and transverse ligaments. It runs from the body of C1 to the internal surface of the occipital bone.
Cervical vertebrae possess small bodies with transverse processes that have a transversarium foramen through which transmit the vertebral artery, vein, and sympathetic nerve fibres. The spinous processes the of cervical vertebrae are bifid (two-pronged).
Thoracic vertebrae have heart-shaped bodies and, with the seventh cervical vertebra, articulate with the ribs at three different sites:
• Each vertebra possesses a superior and an inferior vertebral notch. These structures from adjacent vertebrae form an intervertebral foramen which articulates with the head of the rib. These foramina transmit the segmental spinal nerves
• The transverse processes of each vertebra articulates with the tubercle of the rib.
The lumbar vertebrae have large bodies and transverse processes. The spinous processes are long and angled down and out. The vertebral canal at this level is triangular-shaped.
The sacrum is formed by the fusion of five vertebrae. It is a wide, large, convex bone with four bilateral anterior and posterior sacral foramina through which the sacral nerves exit. The median sacral crest is formed by the remains of the spinous processes (of the fused vertebrae). The sacrum is important in the transmission of the weight of the body through the pelvis to the limbs, via the sacroiliac joints and the pelvic girdle. The upper surface of the sacrum articulates with the lower surface of the 5th lumbar vertebra.
The coccyx is a remnant of the embryonic tail and is the fusion of three to five vertebrae. It articulates with the sacrum. It has no spinous processes, no lamina, and no pedicles.
Intervertebral discs are dense connective tissue structures which absorb loads distributed through the spine. Intervertebral discs form part of the secondary cartilaginous joints (symphyses) between adjacent vertebrae. Each disc comprises two parts—the central, gelatinous nucleus pulposus and the outer annulus fibrosus. Above and below each disc is a cartilage plate centrally, and outer epiphyseal rings, which the annuli insert into. There is no intervertebral disc between C1 and C2 and the most inferior disc is between L5 and S1.
Discs can degenerate (OHCM6 p.396) and become thin (as a result of dehydration). The annulus of a disc may rupture or tear, allowing the nucleus pulposus to herniate (protrude) out of the intervertebral joint. The disc may impinge (OHCM6 p.410) or compress spinal nerves, producing symptoms of pain and neurological deficits.
• The anterior longitudinal ligament attaches to the anterior part of the vertebral bodies and the intervertebral discs. It extends from the inner surface of the sacrum to the anterior tubercle of the atlas (C1) and the occipital bone
• The posterior longitudinal ligament runs within the vertebral canal, attaching to the posterior surface of the vertebrae and the intervertebral discs. It extends from the sacrum to the axis and helps prevent disc herniation
• The supraspinous ligament extends between the tips of the spinous processes of the vertebrae. At cervical levels it becomes the ligamentum nuchae.
• The interspinous ligaments extend between adjacent spinous processes
• The intertransverse ligaments extend between adjacent transverse processes but are only important in the lumbar region
• The ligamentum flava extends between adjacent lamina as a broad elastic band.
The muscles of the back (Fig. 5.60) support the vertebral column and, therefore, the rest of the torso and head. They are divided into three layers—superficial, intermediate, and deep. The intrinsic (deep) muscles cause movements of the vertebral column. The extrinsic muscles (superficial and intermediate) control movements of the limbs and respiration respectively. The musculature of the back also includes muscles which move the head (suboccipital muscles, longissimus capitis).
• The intrinsic muscles of the back are further subdivided into superficial, intermediate, and deep layers. They are important in:
• Control of movements of the vertebral column and the head
• The intrinsic muscles of the back are enclosed by a fascia. In the lower area, it is called the thoracolumbar fascia. The fascia attaches the back muscles to:
• Cervical and lumbar transverse processes
• The superficial layer consists of splenius capitis and cervicis. They play a role in rotation of the head, lateral bending, and extension of the head and neck
• The intermediate layer is formed of erector spinae—the main extensors of the vertebral column. Erector spinae form a prominence either side of the spinous processes
• The deep layer is formed by the transversospinal muscles. From superficial to deep, they are semispinalis, multifidus, and rotators.
Superficial
These are important in the control of the movement of the upper limbs and connect them to the trunk.
Intermediate
Important as an accessory muscle of respiration.
Fig. 5.60 Long extensors of the cervical spine and skull.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p207 (Oxford, 2005). With permission of OUP.
These muscles are involved in maintenance of posture, as well as extension and rotation of the head on C1. They are found in the suboccipital triangle (the area between the occipital bone and the posterior part of C1 and C2). Four muscles are involved:
• Rectus capitis posterior major
• Rectus capitis posterior minor
The back is supplied according to the region:
• Occipital artery (from the external carotid artery)
• Ascending cervical artery (from inferior thyroid artery)
• Deep cervical artery (from the costocervical trunk)
• Vertebral artery (from the subclavian artery)
• Posterior intercostal arteries
• Lumbar and subcostal arteries
• Iliolumbar and lateral sacral arteries (from the internal iliac arteries).
The venous drainage of the back is divided into two different systems:
• External vertebral venous plexus—lies outside the vertebral canal
• Internal vertebral venous plexus—lies inside the vertebral canal, but external to the dura mater of the spinal cord.
The two plexuses communicate freely with the veins in the neck, thorax, abdomen, and pelvis. The basilar and occipital venous sinuses (in the head) communicate with the plexuses via the foramen magnum.
Lymphatic drainage of the back is divided into superficial and deep layers.
• Skin of neck to the cervical lymph nodes
• Trunk (above the iliac crests) to the axillary lymph nodes
• Trunk (below the iliac crests) to the superficial inguinal lymph nodes
• Posterior mediastinal lymph nodes
Posterior rami of the spinal nerves supply the muscles and skin of the back.
Fig. 5.61 Suboccipital muscles, posterior view.
Reproduced from Mackinnon, Pamela and Morris, John, Oxford Textbook of Functional Anatomy, vol 1, p208 (Oxford, 2005). With permission of OUP.
The spinal cord is the main pathway for the transmission of nervous impulses between the brain and the rest of the body. It lies in the spinal canal, surrounded by three meningeal coverings and the cerebrospinal fluid (CSF). The spinal canal is formed from interlocking vertebrae, which protect it.
The spinal cord emerges from the medulla oblongata at the base of the brainstem. It extends (in adults) from the foramen magnum to the level of the intervertebral disc between L1 and L2, where it becomes the cauda equina. Nerves enter and are given off at each level of the spinal cord as dorsal and ventral rami. The nerve root at each segment of the cord is formed by the rootlets of the dorsal and ventral rami as they merge. Dorsal roots contain afferent (sensory) fibres and ventral roots contain efferent (motor and preganglionic autonomic) fibres. The spinal ganglia, located outside the spinal cord at each vertebral level, contain the cell bodies of dorsal root fibres. The ventral grey horns, within the spinal cord, contain the cell bodies of the ventral nerve fibres.
The spinal nerves (8 cervical, 12 thoracic, 5 lumbar, 5 sacral, 1 coccygeal) are formed as the ventral and dorsal roots join together as they exit the vertebral canal via the intervertebral foramina. As a result of greater growth in the vertebral column than the spinal canal during childhood, the nerve roots are increasingly elongated distally and form the cauda equina below L2 in adults. The conus medullaris is a thinning extension of the spinal cord at its most distal end. The filum terminale extends distally from the conus medullaris, attaching to the posterior surface of the coccyx as a strand-like extension of the pia mater.
The spinal nerve divides into the anterior and posterior primary rami almost as soon as it leaves the vertebral canal. These are mixed, containing motor and sensory fibres. The skin and muscles of the back are supplied by the posterior primary rami. The limbs and trunk are supplied by the anterior primary rami.
The spinal cord is covered in three meningeal layers:
• Dura mater is the outer covering of the spinal cord and is a tough fibrous layer. It forms the dural sac and hangs freely in the vertebral canal. It is attached superiorly to the foramen magnum and is continuous with the cranial dura mater. The extradural or epidural space contains connective tissue and separates the dura mater from the periosteum of the vertebral canal. Dural root sleeves are extensions of this covering and extend along the nerve roots out of the intervertebral foramina
• Arachnoid mater forms the intermediate layer and is an avascular fragile membrane which lines the dural sac. The subdural space is an extremely thin layer of serous fluid, separating the dura mater and arachnoid mater. The pia mater is separated from the arachnoid mater by a layer of CSF in the subarachnoid space
• Pia mater is the innermost covering of the spinal cord. It adheres very closely to the cord. It covers the anterior spinal artery and also forms part of the filum terminale. The dentate ligament on either side of the pia suspends it in the dural sac. There are 21 of these ligaments, extending on either side of the cord, halfway between the anterior and posterior nerve roots
• CSF (OHCM8 pp.782, 833) is a clear fluid produced by the choroid plexuses in the 3rd, 4th, and lateral ventricles, and flows into subarachnoid space. The lumbar cistern is a CSF-filled space, continuous with the subarachnoid space, which surrounds the cauda equina and filum terminale below L2.
The spinal cord is supplied by three main arteries which run along its entire length:
• The anterior spinal artery supplies the anterior two-thirds of the cord and lies in the anterior median sulcus of the spinal cord
• Two posterior spinal arteries supply the posterior third and run down the lateral sides of the spinal cord, near the posterior spinal nerve roots
• The spinal cord also has a rich anastomotic blood supply as radicular branches. These originate as branches from the vertebral, intercostal, inferior thyroid and lumbar arteries, and enter the spinal cord via the intervertebral foramina.
The internal vertebral venous plexus (formed by three anterior and three posterior spinal veins) drains venous blood from the spinal cord. The venous sinuses of the cranial dura mater superiorly, and the azygous venous system inferiorly, drain the internal vertebral venous plexus.
The term arthritis describes multiple joint conditions which are characterized by joint inflammation. Affected joints share certain symptoms, including pain, stiffness, and deformity. Either one or multiple joints can be affected, depending on the underlying cause.
Osteoarthritis is the most prevalent joint condition and is about three times more common in women than in men. It is primarily a disease of the elderly, although younger patients can also be affected. Osteoarthritis results from an imbalance between synthetic and degradative processes in articular cartilage (excess degradation, mediated by the cellular component, chondrocytes) although the mechanisms through which this occurs are unclear. In general, osteoarthritis is primary, meaning that the cause is unknown, although it can also be secondary to obesity, joint trauma or instability, or another known cause. There is evidence of genetic predisposition to osteoarthritis in some cases. Joint inflammation characterizes osteoarthritic joints although it is not the primary event.
Osteoarthritis is identified radiographically by a narrowing of the joint space, damage to subchondral bone, and the formation of osteophytes (bony swellings). The primary symptoms are pain, particularly during movement, stiffness, and deformity of affected joints. Osteoarthritis can affect one or many joints but the most common are the joints of the fingers, hips, knees, neck, and lower back.
On a microscopic level cartilage of osteoarthritic joints is first softened then fibrillated and fragmented, and underlying subchondral bone is stiffened. It may also contain calcium crystals (calcium deposition disease) and the zone of calcified cartilage adjacent to subchondral bone (tidemark) may be thickened. Eventually, total loss of articular cartilage can result.
Box 5.1 summarizes the treatments for osteoarthritis.
Like osteoarthritis, rheumatoid arthritis is more common in women than in men. However, unlike osteoarthritis, it usually affects those aged 20–50. Certain genes are linked to an increased incidence of the disease (e.g. HLA DR4). Unlike osteoarthritis, patients with rheumatoid arthritis can experience systemic effects such as pericarditis, pleurisy, and cachexia.
Typically, an autoimmune response is triggered within a joint which results in damage to articular tissues. Inflammatory cells, including monocytes, infiltrate affected joints, and in 80% of affected individuals antibodies (rheumatoid factors) are produced, particularly once the disease has progressed beyond its early stages. These can be detected in the blood. Inflammation results in the release and activation of cartilage degradative enzymes resulting in tissue damage. Rheumatoid arthritis affects many joints, particularly those of the hands and feet. Joint deformation occurs secondary to cartilage erosion.
Box 5.2 summarizes the treatments for rheumatoid arthritis.
 OHCM8 p.550)
OHCM8 p.550)• Gout is the presence of urate crystals in articular tissues, secondary to raised uric acid levels. These can initiate joint inflammation and tissue damage
• Pseudo-gout is a related disorder involving calcium pyrophosphate crystals, rather than urate.
Box 5.3 summarizes the treatments for gout.
Arthritis can also be induced by infectious agents.
• Septic arthritis ( OHCM8 p.546) involves direct infection of a (usually one) joint. Gonococci (secondary to gonorrhoea), staphylococci, and streptococci infections are most common
OHCM8 p.546) involves direct infection of a (usually one) joint. Gonococci (secondary to gonorrhoea), staphylococci, and streptococci infections are most common
• Rheumatic fever occurs following streptococcal infection of the throat and causes generalized inflammation in a number of locations including the joints which are not themselves infected
• Viral infections of the joints can also occur and most frequently involve hepatitis B or C, parvovirus, rubella, Epstein–Barr virus, HIV, or mumps
• Lyme disease occurs secondary to a tick bite and is an infection caused by Borrelia burgdorferi. It involves direct infection of a joint and arthritic symptoms.
Box 5.4 summarizes the treatments for infectious arthritis.
The muscular dystrophies are diseases due to primary dysfunction of the muscle (Fig. 5.62), contrasting with neuropathies where the muscular weakness is due to lack of signal for muscle contraction. Although the muscular dystrophies are rare, they provide an interesting model of disease because the defects in muscle function have been found to be due to dysfunction of specific proteins secondary to mutations in the genes coding for those proteins.
 OHCM8 p.514\)
OHCM8 p.514\)• Due to mutation in gene coding for the protein dystrophin on the X chromosome
• Mutations are usually deletions and dystrophin is usually absent
• Most common form of muscular dystrophy
• Affected males develop normally but, from age of 5 years, develop progressive muscle weakness with use of wheelchair by age of 10 and death due to respiratory failure in 20s.
• Due to mutation in dystrophin but produces abnormal form with some function rather than absence of protein as in Duchenne type
• Later onset than Duchenne type with less muscle weakness
• Many affected individuals have normal lifespan.
All other types of muscular dystrophy are much rarer but are again due to mutations in proteins involved in muscle function (e.g. mutation of gene coding for β-sarcoglycan in type 2E limb girdle muscular dystrophy).
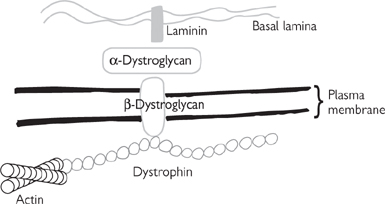
Fig. 5.62 Schematic diagram of muscle proteins which are affected in different types of muscular dystrophy.
The volume of muscle tissue is regulated by the amount and range of use that is made of each particular muscle. Muscle cells do not divide in adults, so there is no increase in the number of cells in response to increased use. However, the volume of the existing cells can increase, as is illustrated, in exaggerated form, by bodybuilders (although there is often some pharmacological assistance in this as well as simple physical training). Similarly, when a muscle is not used, its volume will decrease.
• Physical immobilization of a limb, e.g. in plaster to treat a fracture
• Lack of nerve supply to a muscle, e.g. following trauma to the nerve supply.
Muscle atrophy is completely reversible if the cause is removed within a short time (e.g. a few weeks immobilized in plaster) but if it occurs for longer, then irreversible changes occur (e.g. fatty infiltration of the muscle) and, although some function may return after removal of the cause, the muscle will not return to the same initial level of function.
For prevention and treatment, see Box 5.5.