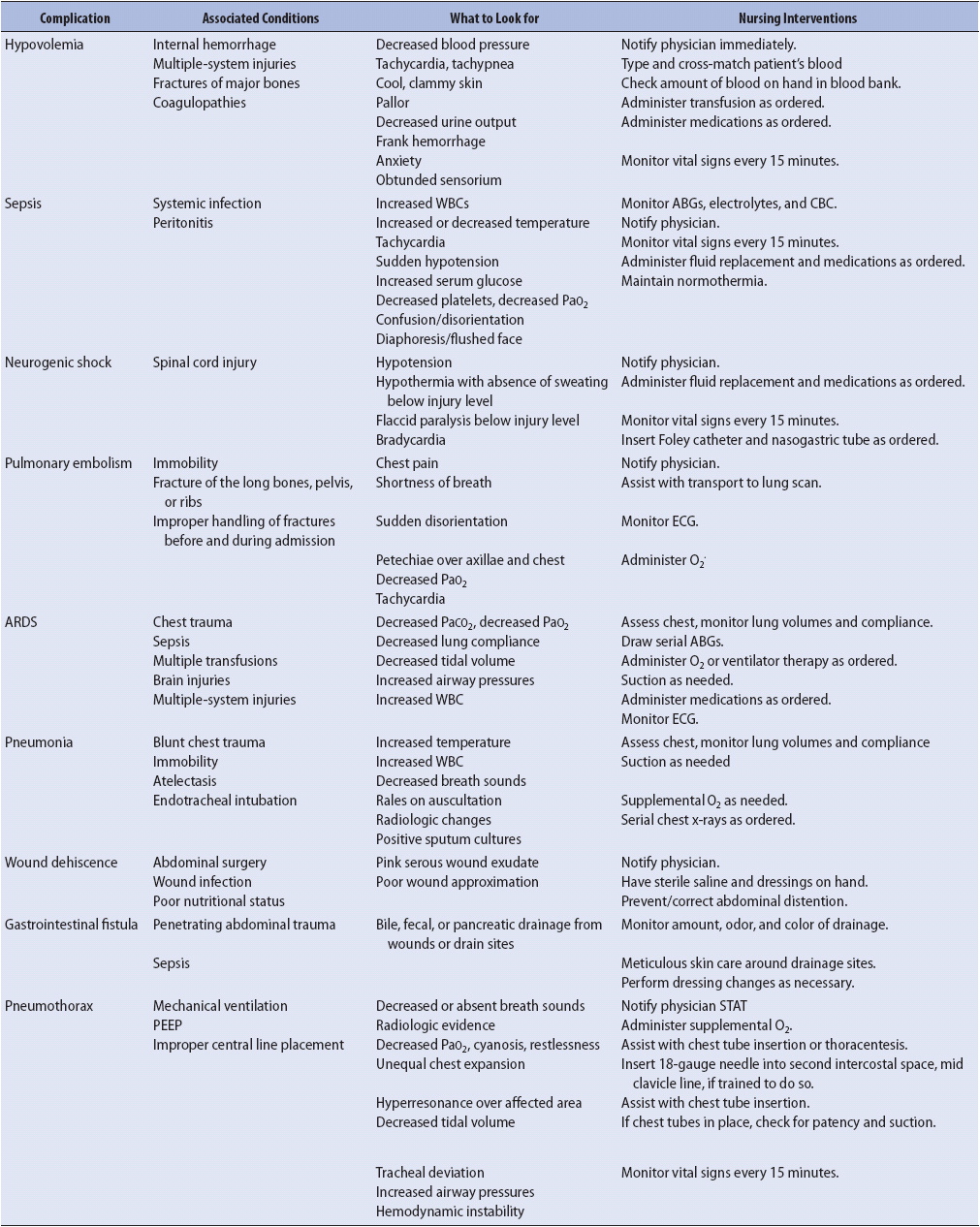
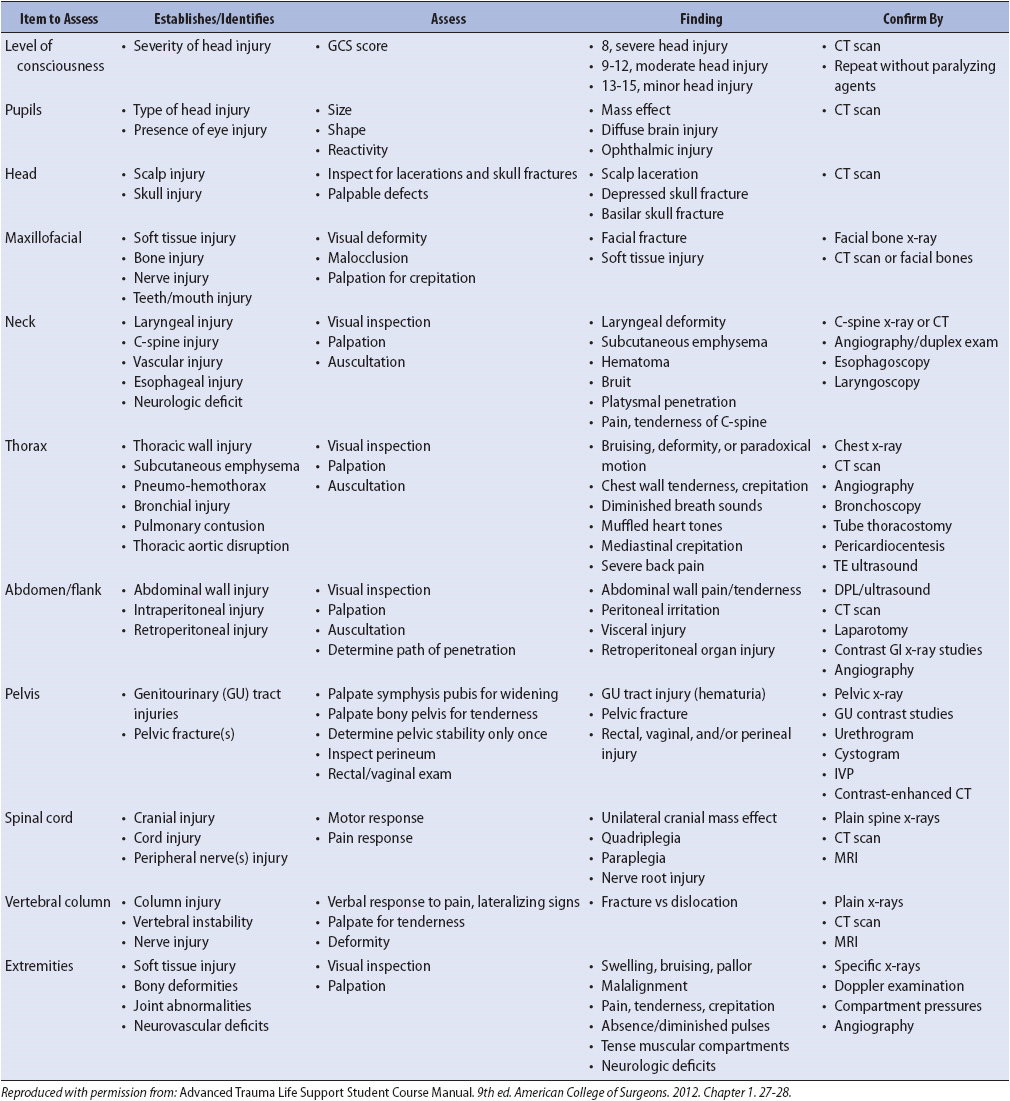
TABLE 17-1. MAJOR COMPLICATIONS IN TRAUMA
KNOWLEDGE COMPETENCIES
1. Describe the mechanisms of traumatic injury and relate them to accurate assessment of overt and covert injuries.
2. Discuss the common physiologic and psychosocial effects on the patient and family because of major traumatic injury.
3. Identify the unique needs of the trauma patient in the progressive care unit.
4. Apply selected management principles to treat trauma patients with thoracic, abdominal, and musculoskeletal injuries.
Trauma is an increasing healthcare problem in the United States. The cost of treating trauma exceeds $400 billion annually. For Americans between the ages of 1 and 44, trauma is the leading cause of death, surpassing cancer and atherosclerosis. Although the death rate is high for this patient population, the disability rate is even greater. This chapter focuses on thoracic, abdominal, musculoskeletal, and pelvic trauma. Although traumatic brain injury and spinal cord injury account for approximately 50% of all trauma deaths, these topics are covered in Chapter 20, Advanced Neurologic Concepts.
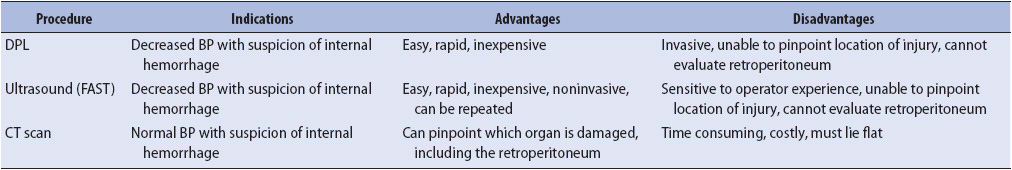
Acutely ill trauma patients are unlike other hospitalized patients and require specialized assessment and monitoring. For the trauma victim, admission to the progressive care setting is sudden and unplanned, without time for psychological preparation or the stabilization of chronic conditions. Trauma patients are often young; however, trauma among the elderly is an increasing problem because of the population’s longer life span. Traumatic injuries may be subtle, and complications are common (Table 17-1). Alcohol or drug abuse plays a major role in the cause of the trauma and subsequent treatment. Rehabilitation is often needed after injury, and a trauma victim’s quality of life may never return to pre-injury status. This is especially true for traumatic brain and spinal cord injuries; however, even in lower extremity trauma, it may take a full year for an individual to return to work. Trauma takes a significant emotional and financial toll on the patient, family, and society.
TABLE 17-1. MAJOR COMPLICATIONS IN TRAUMA
Management of traumatic injury in the initial phases of care occurs in tandem with assessment; for example, the control and insertion of an airway, the administration of fluids, and pain medication may all be provided before the site of bleeding is identified and controlled. One of the most important aspects of assessing the traumatically injured patient is to determine the mechanism of injury, whether blunt or penetrating trauma. Based on this information, an “index of suspicion” regarding specific injuries is developed to ensure that no injuries are overlooked and a trauma patient plan of care is developed.
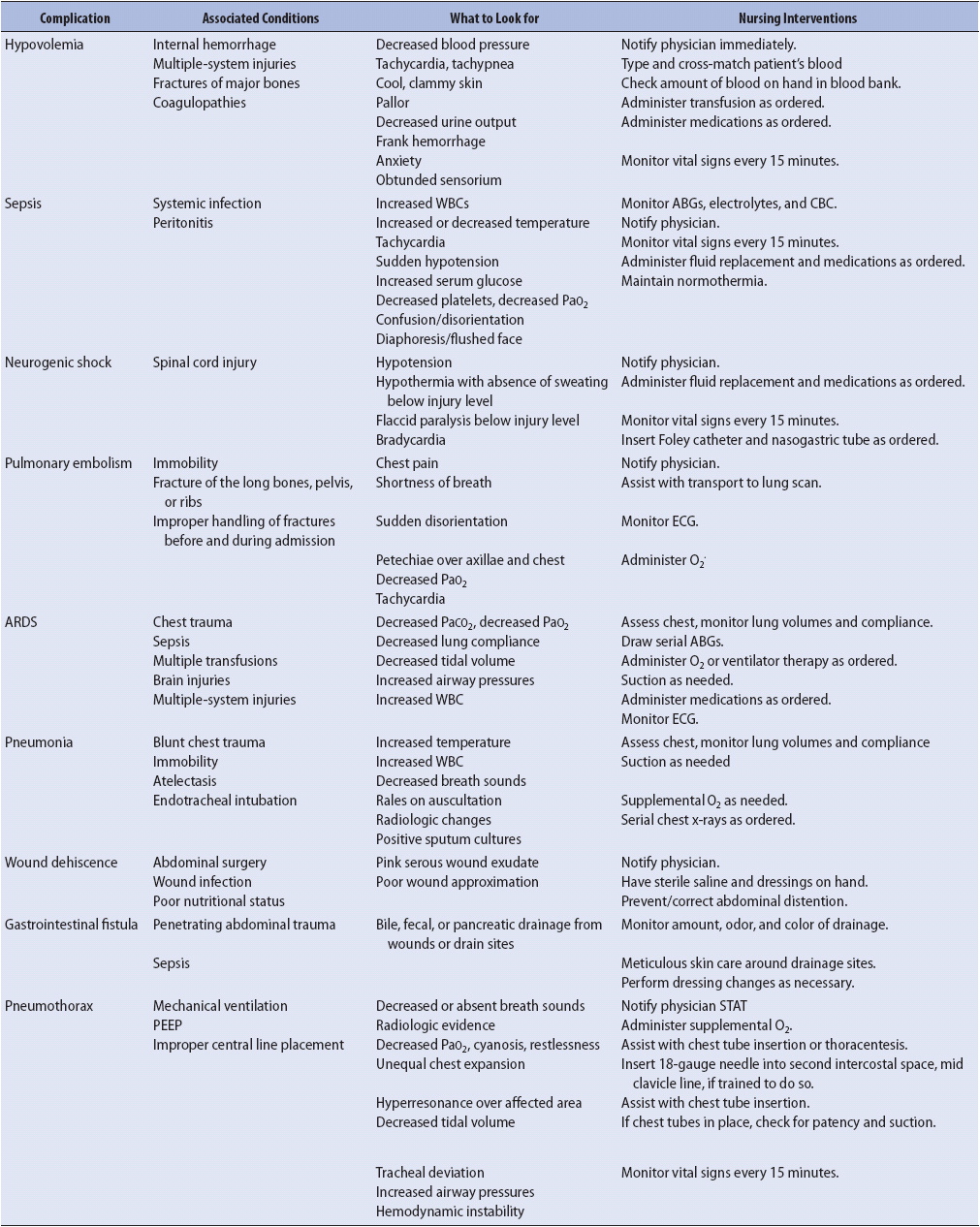
The life-threatening nature of trauma often requires that traditional assessment priorities be changed to address other more serious physical findings (Tables 17-2 and 17-3). The primary and secondary surveys reveal immediate life-threatening injuries and direct the trauma team toward an individualized resuscitation. This approach ensures that common causes of tissue injury are rapidly identified so that appropriate therapeutic interventions can begin. If the patient’s status changes at any time during the secondary survey, the practitioner must return to the primary survey to again review airway, breathing, circulation, disability, and environment/exposure to determine if there has been any physiologic decompensation.
TABLE 17-2. PRIMARY SURVEY
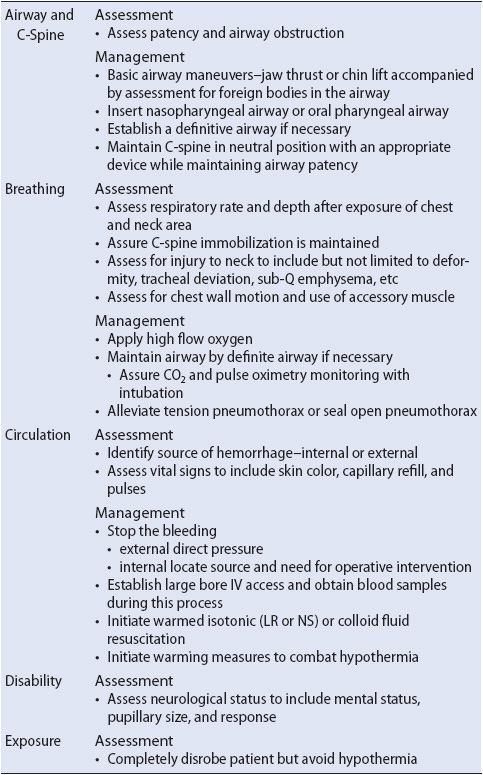
TABLE 17-3. SECONDARY SURVEY
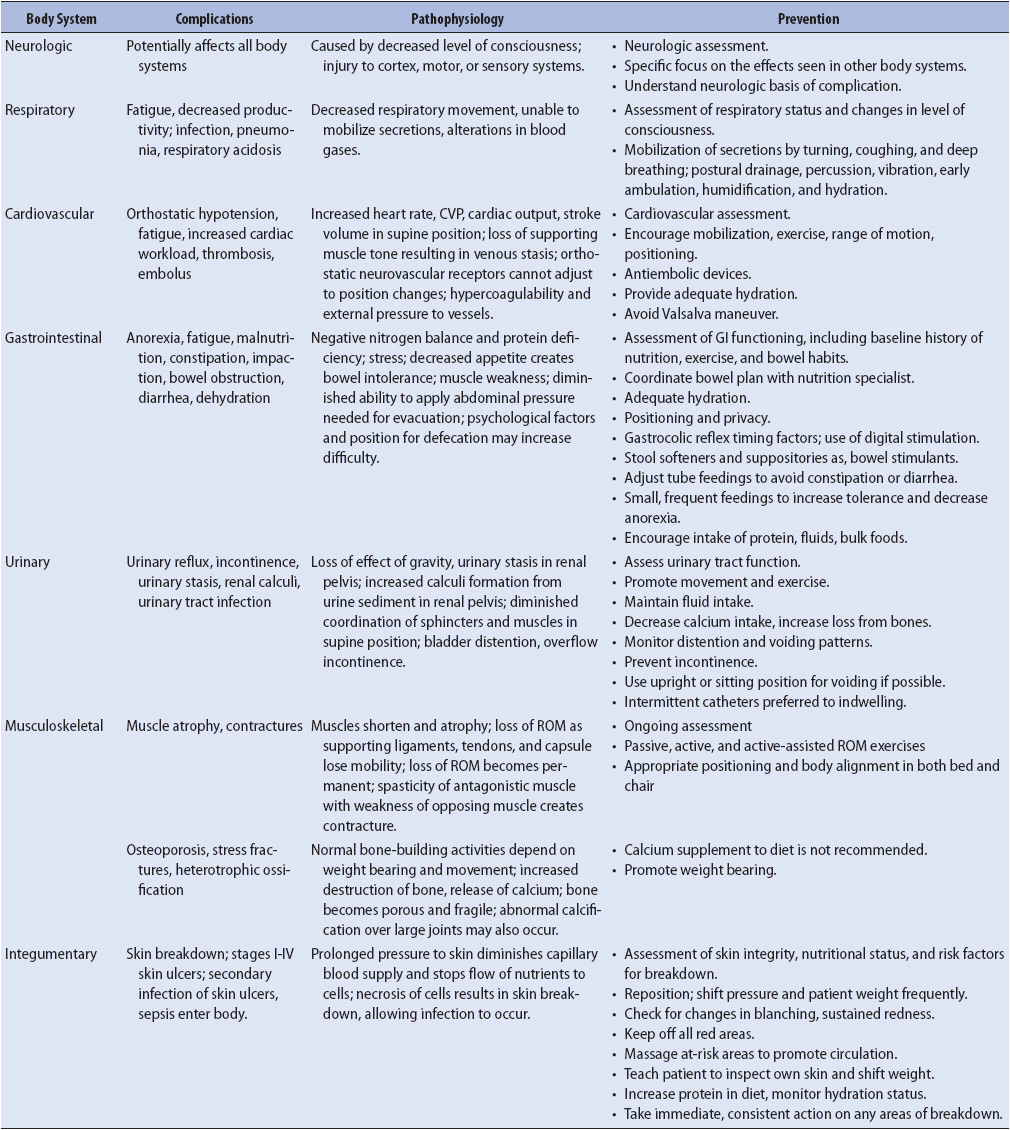
Hemorrhage is of major concern during the primary survey of the trauma patient. Both external and occult bleeding must be considered. Secondary survey diagnostic studies may include diagnostic peritoneal lavage (DPL), ultrasound, and computed axial tomography (CAT) to diagnose occult hemorrhage.
Diagnostic peritoneal lavage is a fast and inexpensive procedure performed to detect free blood in the peritoneal cavity. The test is especially important in the blunt, multisystem trauma patient who is unconscious or those unable to verbalize abdominal pain palpation.
Under local anesthetic, a lavage catheter is percutaneously places into the abdomen. The physician, physician assistant, or nurse practitioner instills and removes sterile fluid from the patient’s peritoneal cavity. A positive tap is defined as the aspiration of greater than 10 mL of blood. If that initial tap is negative, 1 L of saline is instilled and the abdomen is drained by gravity. A minimal fluid return of 250 mL is needed for a sufficient laboratory sample. Hence, only 25 mL of blood must accumulate for DPL to be positive. The lavage is considered positive, and thus the need for surgical intervention is indicated, by 100,000 red blood cells (RBCs)/mm3 or more, greater than 500 white blood cells (WBCs)/mm3, or a positive gram stain for food fibers or bacteria. However, retroperitoneal injuries, such as pancreatic injury, do not show up as positive with a lavage, so vigilant observation of abdominal expansion is required by the nurse.
Ultrasound is used increasingly to diagnose hemorrhage in the trauma patient. Commonly known as the focused abdominal sonograph for trauma (FAST), it can be completed in less than 3 minutes. This noninvasive technique may quickly show injury in the hemodynamically unstable patient. However, the usefulness of ultrasound depends on the experience and expertise of the person performing the study; a DPL may have to be performed for confirmation of hemoperitoneum that was observed by ultrasound.
Focused abdominal sonograph for trauma alone is not acceptable for questionable or borderline findings. For these situations, serial physical examinations coupled with FAST are recommended to better evaluate abdominal injuries. CAT is a good alternative to DPL in the stable trauma patient. CAT scanning continues to be the gold standard for diagnosis of injury if the patient is hemodynamically stable. For a comparison of DPL, ultrasound, and CAT, refer Table 17-4.
TABLE 17-4. INDICATIONS, ADVANTAGES, AND DISADVANTAGES OF COMMON DIAGNOSTIC TESTS FOR BLUNT ABDOMINAL TRAUMA
A cervical spine (C-spine) x-ray is one of the first priorities of assessment after the primary survey. All trauma patients are presumed to have a C-spine injury until all seven cervical vertebrae have been cleared or visualized as intact on x-ray or CAT scan. A cervical collar to immobilize the neck is applied until the C-spine has been evaluated and found to be free of injuries.
Radiographic studies are performed after the primary survey. These studies should not delay resuscitation, but may be essential in determining the extent of injury. Depending on the mechanism of injury, common x-rays may include chest, pelvis, and musculoskeletal studies.
Trauma patients require frequent reexamination to ensure that all injuries are identified and that the patient’s status is not deteriorating. Missed injuries may lead to pain, disability, and increased mortality for the patient. Examples of trauma where repeated assessments by the same provider are recommended include traumatic brain injury and abdominal injuries. Intercranial or occult abdominal bleeding may not be evident initially. Having a high degree of suspicion for traumatic injuries comes from knowledge of mechanism of injury and the specific injuries created by destructive blunt or penetrating forces.
The principles of mechanism of injury give the trauma team insight into the possible injuries sustained by the patient. How an injury occurred, the nature of the forces involved, and suspected tissue and organ damage are all important aspects of mechanism of injury. This knowledge is required when assessing a trauma patient at the scene of the accident and in the emergency department, as well as in the progressive care unit. Knowing this information helps anticipate potential complications.
Injuries result when a body is exposed to an uncontrolled outside source of energy that disrupts the body’s integrity or functional ability. This energy can come from a variety of sources, and can be kinetic, penetrating, chemical, thermal, electrical, or radiating energy. The severity of the resultant injury is determined by several factors: the force or speed of impact, the length of the impact or exposure, the total surface area exposed, and related risk factors such as age, gender, preinjury health, and alcohol/drug ingestion.
Mechanisms of injury are typically divided into two major categories: blunt and penetrating. Blunt trauma is defined as injuries that are not open to the atmosphere, and penetrating injuries are those in which the body has been pierced. Blunt trauma usually results from motor vehicle or motorcycle collisions, assaults, falls, contact sports injuries, pedestrian/vehicle collisions, or blast injuries. Assessment strategies useful in diagnosing blunt traumatic injuries include physical assessment, ultrasound, DPL, CAT scanning, radiographic studies angiography, and blood count, and blood chemistry analysis. Penetrating trauma is commonly caused by bullets or knives in urban areas and by farm or industrial equipment in rural areas.
Knowledge of mechanism of injury provides clinicians with information to determine patterns of injury. These common patterns are helpful when assessing trauma patients who cannot speak to indicate areas of pain. Patterns of injury offer the trauma team an index of suspicion and direction to focus the primary and secondary surveys. Such injury patterns help determine which tests and the sequence of the diagnostic tests needed to identify each of the patient’s injuries; for example, in motor vehicle crashes, the common pattern of injury for the unrestrained driver include head, pelvis, chest, and musculoskeletal areas (eg, hip, ankle, and foot trauma) (Figure 17-1A). Thoracic trauma is often owing to impact with a steering wheel. Other patterns of injuries to unrestrained passengers demonstrate an increased incidence of craniofacial trauma resulting from hitting the head on the windshield (Figure 17-1B). Fractures of the clavicle and humerus are more frequent among passengers, possibly due to the defensive reflex action of raising the arms prior to impact. Similar patterns of injury have been identified for victims of falls and pedestrians struck by motor vehicles (Figure 17-2). Knowledge of these patterns of injuries also helps prevent further damage or complications during the resuscitation efforts; for example, if a patient has sustained a head injury with a high suspicion of basilar skull fracture, a nasogastric tube should not be inserted because it could be passed through the fracture directly into the brain. It should be inserted orally as alternative. A Foley catheter should not be inserted if the mechanism of injury suggests bladder rupture or trauma. A more definitive examination such as the urethrogram or cystogram is warranted.
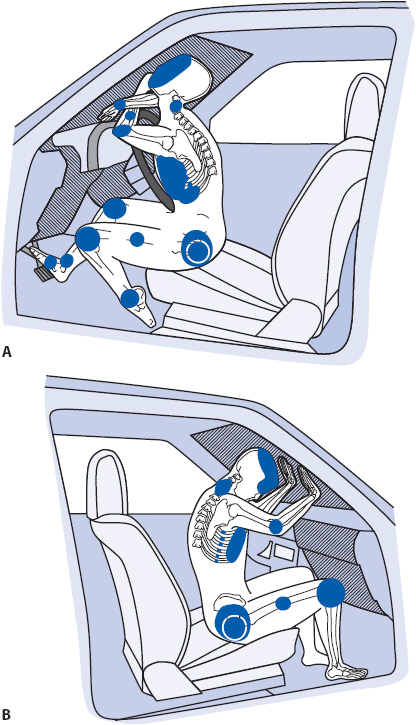
Figure 17-1. Major areas of impact injuries (solid dark areas). The “hostile” contact areas are striped (windshield, steering column, dashboard, and foot pedals). (A) Unrestrained drivers. (B) Unrestrained front seat passengers. (From: Daffner R, Deeb Z, Lupetin A, Rothfus W. Patterns of high speed impact injuries in motor vehicle occupants. J Trauma. 1988;28:499-500.)

Figure 17-2. With an impact to the lower leg from the car bumper or hood, the adult pedestrian rotates and is propelled onto lower leg or hip causing additional injury. (Illustration reprinted with permission from: Weigelt J, Brasel KJ, Klein J. Mechanism of injury. In: McQuillan KA, Makic MBF, Whalen E, eds. Trauma nursing: from resuscitation through rehabilitation, 4th ed. St Louis, MO: Saunders Elsevier; 2009:180.)
Traumatic injury unleashes a cascade of vasoactive mediators, such as various neurohormones, prostaglandins, and cytokines that serve a protective function through the stress response. However, in severe multisystem trauma, these same mediators that help the trauma patient survive the initial injury may prolong the stress response and contribute to complications and even death. This response is best limited by enhancing the patient’s healing ability through attention to physiologic and psychosocial care. Priorities include supporting tissue oxygenation through with the use of oxygen, ventilatory support, and hemodynamic support if necessary. The trauma patient undergoes continuous vital sign monitoring, including pulse oximetry. Pain and anxiety are treated at the same time as injuries are assessed.
Traumatic injury creates fractures, wounds, and crushed tissues that may not be readily visible. Once the ABCs or primary trauma survey has been completed and management begins, the head-to-toe, in-depth assessment, known as the secondary survey, is initiated. In the secondary survey, evidence is accumulated for the detailed diagnosis of multiple trauma and definitive care is planned. A high index of suspicion is needed to link patterns of trauma, mechanism of injury, and physiologic consequences to the traumatic injuries. The progressive care nurse assists in stabilizing the patient with fluids, ventilatory and circulatory support, while also providing emotional support during diagnostic tests. Many times the nurse is responsible for addressing pain control for the patient and the psychosocial needs of the patient and family.
Consequences of traumatic injury include blood loss, tissue destruction, intense pain due to damaged tissues, and altered oxygenation and ventilation. Fluid balance, airway management, aggressive pain control, and wound care are priorities. Stabilization of fractures and surgical repair of injured organs are accomplished in the early operative period. The priority for care in the early phases of trauma is to optimize tissue oxygenation (see Chapter 19, Advanced Cardiovascular Concepts). Although patients in progressive care settings frequently have more than one injured system, a focus on one body system at a time assists in providing an organized management plan.
Thoracic trauma accounts for approximately 25% of all trauma-related deaths and may include injuries created by fractured ribs, blunt cardiac injury, vascular injury, and contused or punctured lung tissue. The most common mechanisms of injury to the chest include blunt trauma (motor vehicle-related injuries) and penetrating trauma from gunshots and stabbings. Common injuries associated with thoracic trauma include tension pneumothorax, hemothorax, open pneumothorax, pulmonary contusion, rib fractures/flail chest, cardiac tamponade, cardiac contusion, or aortic disruption (Figure 17-3).

Figure 17-3. Algorithm: Therapeutic approach to the patient with blunt chest trauma. (From: Mattox K, Feliciano D, Moore F, eds. Trauma. 4th ed. New York, NY: McGraw Hill; 2000:525.)
Injury to the lung parenchyma may cause a tension pneumothorax, which may result in hemodynamic collapse and is therefore a medical emergency. Air collects under positive pressure in the pleural space, collapses the lung, and shifts the heart and great vessels to the opposite side of the chest from the injury causing hemodynamic collapse. Management consists of early detection of the tension pneumothorax and insertion of a chest tube. In emergent situations, if a chest tube insertion is not an option, a large bore angiocath can be inserted into the chest wall at the midclavicular line, second intercostal space to relieve the pressure and tension. Another alternate location is the lateral approach at the midaxillary line. These procedures are known as needle decompressions.
A hemothorax is defined as blood in the pleural space. Fractures to the first and second ribs are considered most serious. If these ribs are broken, one can assume significant force was sustained in the traumatic event, therefore damage to the underlying vessels is possible. An initial chest x-ray demonstrating a widened mediastinum often confirms this suspicion of hemothorax. If the hemothorax is large enough and the patient is experiencing respiratory difficulty, a chest tube is placed to drain the hemothorax. If the patient is hemodynamically unstable, the physician may need to perform an open thoracotomy to control the bleeding.
An open pneumothorax is present when there is passage of air in and out of the pleural space. This usually occurs when there is a penetrating injury to the chest wall by either a gunshot or stab wound. A dressing may be applied to the open sucking chest wound with careful attention to taping only three sides of the dressing. If the dressing is made occlusive, a tension pneumothorax may occur. The patient needs a chest tube placed in the affected side.
Pulmonary contusion is injury to the lung parenchyma, which commonly occurs after blunt injury to the chest. A pulmonary contusion may lead to alveolar capillary membrane disruption. Depending on the severity of the contusion, hypoxemia occurs, which may worsen several days after the injury, progressing to respiratory failure and acute respiratory distress syndrome (ARDS). Pulmonary contusions are difficult to identify and diagnose during the initial trauma resuscitation because clinical findings may not occur until several hours after the injury. This injury is an example of when an index of suspicion and knowing the mechanism of injury assists the progressive care nurse to anticipate pulmonary complications such as hypoxemia progressing to respiratory failure and ARDS.
Fractured ribs are also common in blunt trauma. Fractured lower ribs can damage the liver or spleen, and upper rib fractures may puncture lung tissue. All patients with rib fractures are suspected of having a pulmonary contusion. A flail chest may occur when three or more adjacent ribs are fractured in two segments, creating a “floating segment” that may puncture the lung and compromise effective ventilation efforts. Diagnosis of a flail chest is made by observing inward movement of the chest during inspiration and outward movement during expiration. This injury is best assessed when the patient is breathing spontaneously. With this kind of injury there is a paradoxical motion of the chest wall which results in hypoxemia. Due to pain, the patient is often unable to take a deep breath leading to atelectasis and further compromising oxygenation and ventilation. Pneumonia and/or respiratory failure may ensue if not treated.
Blunt cardiac injury may result in damage to the myocardium, coronary arteries, or structures of the heart (septum or valves) as a result of blunt force to the chest. These injuries might be subtle and difficult to diagnose but should always be a matter of concern when a patient has sustained chest trauma. The transthoracic echocardiography, 12-lead ECG and biochemical markers (troponin levels) are used to assist in the identification of myocardial injuries. Dysrhythmias are common in these patients. Sinus tachycardia, atrial fibrillation, and premature ventricular contractions are most common. In contrast ventricular tachycardia and fibrillation are unfortunately more common if the area of myocardial damage is large.
Cardiac tamponade is a potentially life-threatening complication of both blunt and penetrating chest trauma. The pericardial membrane (sac) is normally stiff and noncompliant. Bleeding into the pericardial sac (effusion) causes compression of the heart, which then compromises cardiac function and cardiac output. The rate at which fluid accumulates around the heart in the pericardial sac determines whether the effusion will lead to cardiac tamponade or compensation (stretching of the sac and accommodation). A rapid accumulation of blood does not allow the pericardial sac to stretch and the tamponade may lead to pulseless electrical activity and/or cardiogenic shock.
Traumatic aortic disruption is a surgical emergency and the most common cause of immediate death in the thoracic trauma patient population. A clinician with a high index of suspicion and knowledge of mechanism of injury, such as high-speed motor vehicle collision, will identify this injury earlier and potentially improve the outcome. Historically, the gold standard for diagnosis was angiography. But with the modern advances in bedside echocardiography and the quickness of the CAT and MRI imaging, these tests frequently allow for a confident diagnosis without the need for angiography. A widened mediastinum is typically seen on chest x-ray. The survival rate of the patient is directly related to how quickly this injury is diagnosed and the patient is taken to the operating room.
Management of the patient with trauma to the chest must be individualized to the patient and includes several basic principles: ventilatory support to prevent hypoxemia; monitoring chest tubes for drainage; providing optimal pain control and positioning to promote adequate oxygenation/ventilation, to decrease complications of immobility, and to promote wound healing; and limiting the risks of infection.
The goals for ventilatory support of the trauma patient are the same as the ventilatory goals for any patient in the progressive care unit. Management focuses on improving oxygenation, correcting acidosis, easing the work of breathing and decreasing the risk of ventilator associated conditions (VAC). Ventilatory therapy may be definitive or supportive, depending on the patient’s injury and requirements. Definitive care for a flail chest may include the use of the ventilatory support to stabilize the chest wall. Supportive ventilatory care is imperative in the patient with a pulmonary contusion who exhibits signs of ARDS. The nurse caring for the trauma patient must be comfortable with the modes of conventional mechanical ventilation and have an awareness of some of the nonconventional ventilatory techniques (see Chapter 5, Airway and Ventilatory Management).
Chest tubes are inserted for patients with chest wall injuries and punctured lung tissue and those requiring thoracotomy. Care of the patient with chest tubes includes observing for drainage characteristics, signs of a resolving air leak, and prevention of infection. Meticulous sterile technique, insertion site care, and drainage system set up are key components of chest tube management. Trauma patients may have draining wounds and suture lines adjacent to the chest tube site, which can make dressing changes more complicated. Infection surveillance, prevention, and assessment are essential nursing functions for all trauma patients.
Pain control, both systemic and local, is needed and may even preempt the need for mechanical ventilation in patients with milder degrees of thoracic trauma; for example, when patients are able to breathe deeply and cough effectively, smaller airways remain open, atelectasis is avoided, and healing can occur. Patient-controlled analgesia (PCA), epidural narcotic infusions, or local anesthetics can be used for aggressive pain control in the trauma patient to allow for enhanced pulmonary function exercises and avoid the need for mechanical ventilation.
Patients report that chest tubes, suctioning, and turning are all extremely painful. Managing a patient’s pain aggressively is not only a humane concern, but it also allows the patient to focus mental and physical energy on healing. Pain can be controlled through narcotics that act centrally, locally, or regionally, and through drugs that act at the periphery to interrupt the painful stimulus (see Chapter 6, Pain, Sedation, and Neuromuscular Blockade Management and Chapter 7, Pharmacology). Nonpharmacologic approaches can also operate at the central level through cognitive distraction or relaxation, and peripherally by using positioning or application of heat and cold.
Patient-controlled analgesia gives the patient control to request pain medication at a preset time interval. Epidural PCA is used with success in patients with rib fractures and may decrease the need for mechanical ventilation, an important benefit in older trauma patients. Vigilant nursing care is essential because the epidural catheter may migrate and not provide adequate pain relief. A patient’s report of pain relief needs to be requested by the nurse at hourly intervals initially; it is the only reliable measurement for pain.
The progressive care nurse will have to rely on assessment data to determine the need for antianxiety and analgesic medication administration. If there is a perception, the nurse perceives the injury as painful, and the patient is unable to communicate or physiologically respond to painful stimuli due to drugs (beta-blockers, etc) pain medication should be encouraged based on that perception.
A variety of nonpharmacologic pain-reducing strategies are useful in patients with trauma, and the nurse needs to combine these with drug therapy for maximal gain. Because narcotics have side effects, combining them with a nonsteroidal anti-inflammatory agent and a cognitive intervention may offer the patient the best pain reduction possible. Cognitive interventions for pain includes relaxation, guided imagery, music therapy, pet therapy, or hypnosis. Clear documentation of what strategies or combinations work best for the individual is needed. This approach requires an established communication system between patient, nurse, nurse practitioner, and/or physician. Anxiety and sleeplessness contribute to the pain response and should be addressed by asking the patients how they typically try to relax and by eliminating as much environmental noise as possible. Encouraging rest and sleep and limiting patient interruptions provides better pain management.
Early mobilization of the trauma patient assists in promoting oxygenation and ventilation, and other complications of immobility. This includes positioning the patient in and out of bed. Information obtained from daily chest x-ray results is essential for accurate positioning of the patient. Positions to be considered include: sitting, prone, and lateral decubitus. The lateral decubitus position with the good lung down is especially important to maximize oxygenation if there is unilateral lung disease or injury to one side of the chest. An example of how the concept of therapeutic positioning can be used by the nurse is to position the patient and observe chest excursion, respiratory rate, pulse oximetry, peak inspiratory pressures, and if applicable, hemodynamic data for improvement. Continuous lateral rotation and/or prone positioning beds may be helpful for selected injuries and or conditions.
Trauma to the abdomen may occur to organs in three distinct abdominal regions: peritoneal cavity, retroperitoneum, and pelvis. The trauma will be directly related to the mechanism of injury and the anatomical location that was impacted. The organs most affected by blunt abdominal trauma are the spleen, liver, and kidneys. From penetrating mechanisms, the liver and intestines are more commonly injured (most penetrating trauma is anterior). The types of injuries sustained could be organ contusions, lacerations, fractures, vascular disruption and hemorrhage, and crush-type tissue damage. Abdominal trauma is frequently not as overt on primary and secondary assessments as other injuries, but it is frequently more life threatening. Physical examination, the presence of pain, FAST, and the abdominal CAT scan are the main methods used to diagnose potential injuries and are the primary tools used to determine if the patient needs to go directly to the operating room or should be closely monitored. Vigilance in nursing assessment for overt changes and observance of trends are the keys to identifying abdominal injuries. The MRI, DPL, and angiography also might be used for assessment.
The FAST and the abdominal CAT scan are two diagnostic tools used in conventional trauma assessment. FAST exams are rapid, noninvasive, and can be repeated multiple times throughout the resuscitation period. Abdominal CAT scanning requires a hemodynamically normal patient and is more costly than FAST exams. Historically, if the patient was unable to reliably confirm or deny the presence of abdominal pain, a DPL would be performed. For patient safety during a DPL a decompressed bladder and stomach is necessary. The entry into the abdomen with the needle increases the likelihood of injury.
To perform a DPL, a catheter is inserted just below the umbilicus and normal saline is infused. The bag is then lowered below the abdomen and the fluid allowed to drain out. If the fluid does not come out or it is bloody or cloudy, there is a high probability of abdominal trauma. A DPL cannot discover a retroperitoneal bleed.
Damage to the spleen is one of the most frequently encountered blunt abdominal trauma injuries. Depending on severity of splenic injury, interventions range from non-operative observation, embolization angiography, and bedrest for mild lacerations to removal of a massively ruptured spleen. Liver trauma runs the spectrum from minor injury to severe laceration, requiring operative repair and packing. The bowel, pancreas, and kidneys can be directly injured or sustain secondary injury as a result of poor perfusion and/or inflammation during the trauma, resuscitation, or critical care phase of recovery.
Typically, presenting signs and symptoms in abdominal trauma include pain and hypovolemia. Complications from abdominal trauma are directly linked to the function of the gastrointestinal tract and include metabolic/nutritional alterations, infections such as peritonitis, and pancreatitis. Patients may require extensive dressing changes if the wound is open or requires frequent surgeries for staged repair of the abdominal organs.
Selected principles of caring for the patient with abdominal trauma include monitoring for bleeding, infection prevention and management, and initiating early (within 24-48 hours) nutritional support.
Acute hemorrhage is commonly addressed during the primary survey and frequently requires surgery. Occult bleeding may not be initially evident and later be discovered by the acute care nurse. Common abdominal injuries that may not initially exhibit signs and symptoms of bleeding include liver laceration, splenic fractures, and slow retroperitoneal bleeds.
Spleen injuries were historically treated with splenectomy. The conventional wisdom is to preserve the spleen if possible. Splenorrhaphy, embolization repair of the spleen, or watchful waiting is increasing in popularity. The goal is to allow the spleen to heal and preserve the valuable immunoprotective function. If splenectomy is indicated due to massive injury, patients are given polyvalent pneumococcal vaccine within 72 hours after surgery to prevent infection with pneumococci. These patients will have immune compromise the rest of their lives. Management also includes a minimum of 3 days of bedrest, monitoring for rebleeding, and interventions to prevent the complications of immobility.
Abdominal trauma victims are at high risk for infection even when surgery has not been performed. One of the major nursing care priorities (after airway and bleeding) in all trauma patients is prevention, assessment, and management of infections. Traumatic wounds can be simple lacerations or abrasions from a motor vehicle crash or complex open abdominal surgical wounds that require packing and frequent trips to the operating room. Care for the patient with a large abdominal wound is directed by the type of wound (open or closed) and the degree of intracompartment contamination due to the injury and surgery. Careful consideration of antimicrobial therapy must also be considered with contaminated wounds. The dressing changes are frequently performed by the acute care nursing staff, so assessment for signs of infection as well as wound healing is essential during these dressing changes. Premedicating the patient or timing dressing changes around pain medication administration is another important role of the nurse providing holistic care. These patients frequently may have multiple sources of infection. The presence of a central line, Foley catheter, ET tube, nasogastric tube, chest tube, and peripheral IV all increase the risk of hospital-acquired infection. Sepsis is always a risk for any trauma patient and that risk is increased with abdominal trauma victims.
Nutritional support in the trauma patient is multifactorial and an integral part of trauma care. Management focuses on the route and timing of nutritional support. Other considerations include composition of nutrient formulation, assessment of laboratory tests that measure nutrition, and enteral verses parenteral feedings. Trauma patients have increased metabolic needs due to a hypermetabolic stress response caused by severe injuries, wound healing, and/or sepsis.
Enteral nutrition is encouraged whenever possible at the earliest time after injury. Even a small amount of nutrition delivered via tube feeding to the gut is believed to be beneficial. A variety of metabolic derangements in the hypermetabolic trauma patient make nutritional support an early imperative. Insertion and maintenance of a small-bowel feeding tube, percutaneous gastrostomy tube, or jejunostomy tube is often required after injury until the patient can be orally fed. Total parenteral nutrition is recommended only if the gastrointestinal tract is unable to tolerate adequate nutrients. Accurate nutritional assessment conducted in collaboration with the nutritionist is essential, as trauma patients are at risk of complications from overfeeding as well as underfeeding. Diarrhea, inappropriate withholding of tube feedings, and the potential for increased aspiration are issues that need to be addressed for trauma patients (see Chapter 14, Gastrointestinal System).
Trauma to the musculoskeletal system accounts for approximately 70% to 85% of polytrauma injuries. Patients in the progressive care setting with extremity or pelvic fractures often have other injuries due to the significant physical impact to the body. Motor vehicle trauma, falls, sports injuries, and industrial trauma are all frequent causes of musculoskeletal trauma. Victims of motorcycle crashes frequently have severe fractures with extensive soft tissue damage. Massive blood loss, edema of tissues, tissue destruction, and pain accompany musculoskeletal injuries.
Compartment syndrome is a serious complication of extremity trauma as a result of contused tissue swelling in a specific muscle compartment (Figure 17-4). This may lead to lack of perfusion and nerve compression in the area. Muscle compartments are located in the forearm, leg, hand, foot, thigh, abdomen, and chest. The nurse assesses for signs of compartment syndrome and performs early and repeated neurovascular checks. However, neurovascular assessment of the five P’s (pain, pallor, pulselessness, paresthesia, paralysis) may not provide accurate early assessment of rising compartment pressures. Nursing management consists of immobilization and extremity level with the heart or below. Elevation of the extremity can worsen condition. Assessment of compartment pressures requires the use of a specialized needle that is inserted directly into the tissue compartment. The needle/catheter is attached to a transducer and the compartment pressures are evaluated and monitored. Even open fractures may have significantly increased compartment pressures (normal pressure 0-8 mm Hg). If the compartment pressures are found to be high, a fasciotomy will be preformed to relieve the pressure. A fasciotomy entails surgically opening the skin and fascia to relieve the pressure in a muscle compartment and is the treatment of choice for compartment syndrome. The primary goal of fasciotomy is to improve perfusion and minimize distal tissue damage from ischemia.
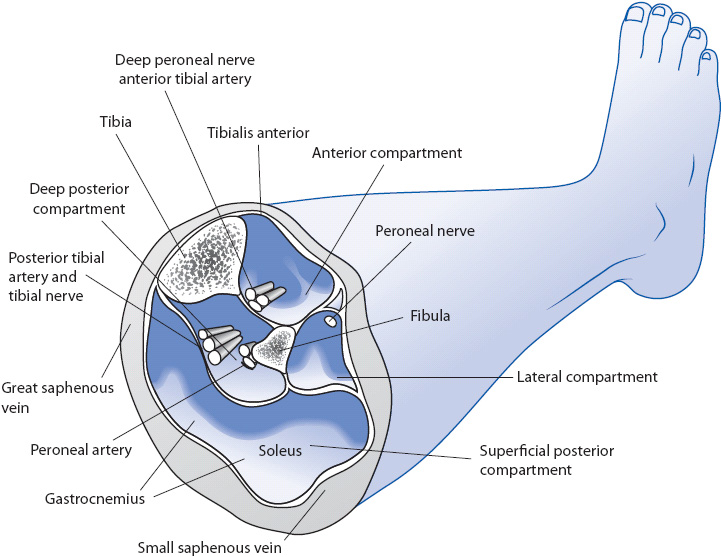
Figure 17-4. Compartments of the lower leg. (Illustrated and used with permission by David Hayes, Fultan, MD, 2009.)
Management of extremity trauma focuses on early stabilization of fractures to prevent further tissue damage, infection, bleeding, and disability. Complications from musculoskeletal trauma include immobility, which can lead to increased incidence of pulmonary emboli, fat emboli, deep venous thrombosis, and pressure ulcers. Pain control to promote mobility, and assessment of neurovascular status are key components to managing these patients (Table 17-5).
TABLE 17-5. PHYSICAL COMPLICATIONS RELATED TO IMMOBILITY COMMONLY SEEN IN TRAUMA PATIENTS
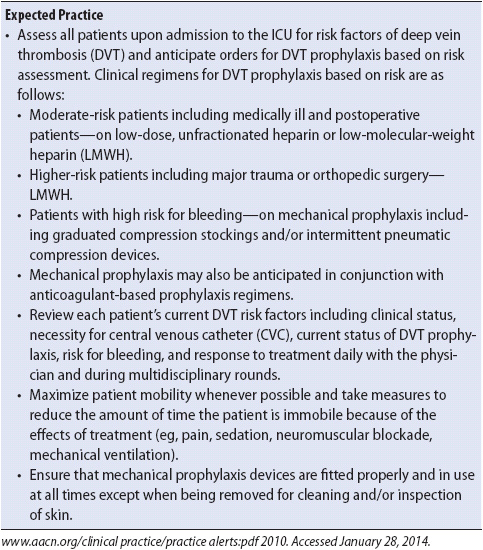
Fractures are repaired early after a traumatic injury to decrease bleeding and to limit immobility and its complications (eg, pulmonary embolism). Guidelines for the management of venous thromboembolism for trauma patients include thromboprophylaxis and mechanical prophylactic devices, such as sequential compression devices (Tables 17-6 and 17-7).
TABLE 17-6. EVIDENCE-BASED PRACTICE: MANAGEMENT OF VENOUS THROMBOEMBOLISM IN TRAUMA PATIENTSa,b
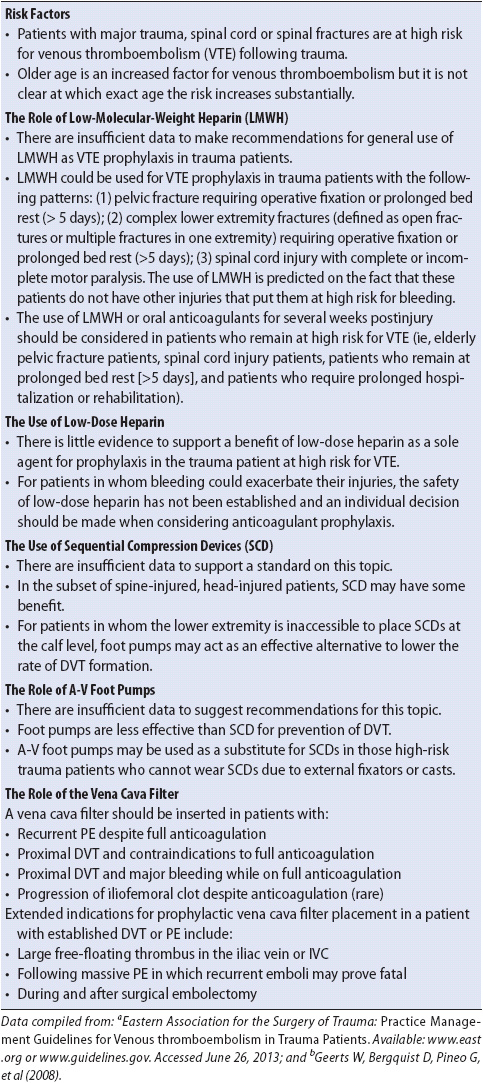
TABLE 17-7. AACN PRACTICE ALERT GUIDELINES FOR DEEP VEIN THROMBOSIS PREVENTION
Fractures are repaired early after a traumatic injury to decrease further bleeding and to limit pulmonary embolism complications. External fixation is used for pelvic fractures and lower limb fractures. Frequent sensation, movement, and vascular checks on affected extremities are essential. If the presence of pulses is in doubt, Doppler ultrasound should be used at the bedside.
Pain control is best achieved with an individualized strategy of medications and nonpharmacologic therapies. Patients respond best when strict attention is paid to pain control and their own unique coping style is used. Patients are expected to move in the bed and get out of the bed as soon as possible after an injury. Titrated pain medication is required to achieve this goal using PCA or continuous infusion. Nurses need to determine patient anxieties regarding the trauma and promote adequate sleep and rest. Sleep deprivation from a noisy environment, constant worry, and needless pain only makes the patient perceive a more intense pain.
The key to survival for patients with multiple trauma is to limit the extent of complications experienced and increase the delivery of oxygen to the tissues during the initial phase of resuscitation. In the history of trauma as a clinical specialty this has been called the “golden hour.” The resuscitation goal is to prevent tissue oxygen deprivation due to hypoperfusion and identify and eliminate the cause of problem. Shock, by definition, occurs when cellular oxygen delivery does not meet oxygen demands, which leads to cellular hypoxia. When adequate oxygen and blood flow are provided during the resuscitative phase of trauma, the likelihood of shock and hypoperfusion complications decrease. Heart rate and blood pressure are not considered adequate parameters to judge the effectiveness of resuscitation, because they indicate only the body’s compensation for the stress of trauma and not real-time tissue oxygenation. Appropriate measures to evaluate resuscitation should focus on assessing tissue oxygen delivery, including oxygen transport, delivery, and utilization. Evaluation of base deficit as an indicator of oxygen delivery at the cellular level is invalid. Base deficit is a good prognostic indicator of the effects of the general resuscitation efforts but not at the cellular level. Therefore, as the base deficit rises, a lactic acid test should also be done to assess perfusion at the cellular level (see Chapter 19, Advanced Cardiovascular Concepts). Serum lactate rises with inadequate oxygenation and is an additional diagnostic indicator of the adequacy of reperfusion and oxygen delivery. To preserve adequate blood flow in the acutely injured trauma patient, permissive hypertension may be used. In contrast, permissive hypotension is based on the concept that resuscitation to attain normal blood pressures may increase bleeding from a site that has already “clotted” through the normal clotting cascade process. In this case large volumes of blood are not encouraged.
Common complications of trauma are infection/sepsis,
ARDS, and systemic inflammatory response syndrome (SIRS) (see Chapter 10, Respiratory System, and Chapter 11, Multisystem Problems). Patients with sepsis and SIRS experience a persistent inflammatory response, which can lead to acute lung injury and multiple organ dysfunction syndrome (MODS). Multiple organ dysfunction or failure begins during hypoperfusion and shock phase, and if reperfusion is not quick or adequate enough, the organs sustain ischemia, inflammation, injury, and possibly infarction. The clinical presentation of organ dysfunction may have a rapid onset or take days to weeks to present. It can be assessed by the critical care nurse as signs and symptoms of ARDS, pancreatitis, ARF, hepatic insufficiency, or any organ failure. Delivering oxygen to the tissues by maintaining increased blood flow during resuscitation and early acute care phases is believed to decrease the length of hypoperfusion and anaerobic metabolism and these often lethal complications.
Achieving adequate oxygen delivery to the tissues requires oxygen, hemoglobin, and sufficient cardiac output to deliver them to the organs and cells. This is typically accomplished with massive fluid and or blood resuscitation. Massive transfusion is defined as the administration of more than 10 U of blood (whole blood or packed red blood cells) within 24 hours, replacing the patient’s total blood volume. Trauma patients are at risk of experiencing significant complications after massive fluid/blood administration. Hypothermia coagulopathy, acidosis, electrolyte imbalances, transfusion-related acute lung injury (TRALI), transfusion-associated circulatory overload (TACO), transfusion-associated immunomodulation (TRIM–a down regulation of immune function or immunosupression), and the cause of posttransfusion infections have all been attributed to massive fluid or blood replacement. Monitoring for and treating these complications are essential during the critical care phase of trauma patient care.
Patients with trauma have an increased incidence of ARDS (see Chapter 10, Respiratory System). Precipitating factors for ARDS in the trauma patient include direct or indirect injury to the lungs. Examples of direct injury include smoke inhalation, rib fractures, or large pulmonary contusions. Indirect injury may be due to sepsis, massive fluid resuscitation, and prolonged hypoperfusion states (shock) which may all lead to an inflammatory insult and alveolar infiltration.
Standard treatment for ARDS includes mechanical ventilation, oxygen titrated to maintain Pao2 above 60 mm Hg, and ventilatory modes and methods to recruit closed alveoli and decrease lung injury. In addition to mechanical ventilation, another method to improve oxygenation is positioning for optimal ventilation and perfusion. This is a unique challenge for acutely ill trauma patients because their traumatic injuries may preclude many positions; for example, the patient with an unstable pelvic fracture, a spinal cord injury, or lower extremity fractures may be difficult or impossible to turn. Meticulous nursing care to prevent ventilator associated complications (VAC) is a priority for all trauma patients receiving mechanical ventilation.
Trauma patients are at high risk of developing an infection and potentially sepsis. This is because of the nature of the injury, the environment in which the injury occurred, the nonsterile conditions in which invasive devices may have been initially placed, and the multiple invasive procedures, including surgery, necessary for trauma resuscitation and management. The procedures preformed during resuscitation are at best undertaken under clean conditions.
The classic signs and symptoms of infection are sometimes difficult to isolate in a recovering trauma patient. Fever, tachycardia, elevated white blood cell count, hypoglycemia inflammation, pain, and a hyperdynamic state are classic indicators of infection and sepsis. These assessment parameters are also common after injury, resuscitation, and during the healing process due to the stress response on the immune system. The classic rule in trauma care is that there is an infection—it just needs to be found and treated. When clear identification of an infectious source is elusive, a finding of elevated C-reactive protein and procalcitonin levels are sometimes considered confirmation that an infectious source exists. Meticulous attention to sterile technique and hand washing is essential in this vulnerable patient population.
Identification and management of SIRS requires knowledge of the underlying inflammatory process (see Chapter 11, Multisystem Problems). Assessment criteria for SIRS includes two or more of the following: temperature greater than 38°C or less than 36°C, heart rate greater than 90 beats/min, respiratory rate greater than 20 breaths/min, PaCO2 less than 32 mm Hg, and white blood cell count greater than 12,000/mm3 or less than 4000/mm3. The systemic inflammatory response has occurred because of direct injury to tissues/organs and lack of oxygen delivery (hypoperfusion) during the shock state. These circumstances lead to the release of biological mediators from injured tissue/cells, which cause an intense systemic inflammation, vasodilatation, and increased membrane permeability (edema, leaky tissue). The cardiopulmonary changes typical in SIRS include high cardiac output, decreased systemic vascular resistance, and elevated oxygen requirements and consumption.
Goals for managing the patient with SIRS are to provide the essentials such as oxygenation and nutrition, limit known stressors such as pain and fever, and support organ system function. The delivery of oxygen and nutrients requires an adequate cardiac output, oxygen-saturated hemoglobin, and an environment (pH) in which the cells can extract and utilize the delivered oxygen. Fluid resuscitation, vasoactive and inotropic drug administration may be necessary to maximize oxygen delivery during the SIRS phase.
The individual’s response to SIRS may be prolonged and destructive, leading to MODS. As organs begin to dysfunction and fail, treatments such as maximal ventilatory support and hemodialysis may be necessary. Mortality remains high for MODS, requiring increased attention to prevention of early following trauma hypoperfusion. Limiting the initial shock (hypoperfusion) state decreases the likelihood of SIRS and therefore MODS. In trauma care, the multidisciplinary team’s interventions in the first 24 hours of injury often determine survival.
Acute illness places many stresses on patients and families, resulting in unique psychosocial implications. Trauma injury is by nature unexpected. It typically affects young, healthy individuals and can launch both the patient and family into a cycle of chaos and crisis. Common responses to trauma include anxiety, fear, grief, loss, guilt, depression, denial, sleeplessness, and hopelessness.
Fear begins immediately as the awake trauma patient is transported from the scene. Fear is related to the unknown, the specifics of the injuries, and impact on the patient’s future, including body image, family, and career. Loss typifies the experience of trauma and can be characterized as loss of physical functioning, loss of quality of life, or even loss of significant others due to the traumatic event. Guilt may ensue as the patient may perceive responsibility for the event (directly or indirectly) and this can be overwhelming. Depression and denial are common coping mechanisms used during personal crises and may be exhibited in a variety of ways by trauma victims. It should be noted that although the injuries were sustained by the patient, the family members, and family structure frequently are also traumatized.
Monitoring the patient’s response to injury is as much the responsibility of the nurse as monitoring the patient’s blood pressure. As there are long-term physiologic effects of a low blood pressure (shock), so are there long-term psychological effects of unmet or unidentified emotional needs. There are also psychoneuroimmunologic in responses that can impact the physical recovery. The emotional response to injury should be assessed. Talk to the patient and listen to their responses and perceptions. Help them to identify and articulate their concerns and fears.
Fear creates anxiety in the trauma patient, and unrelieved pain may worsen anxiety. With the intense monitoring and frequent care interruptions in the progressive care environment, sleep may be impossible. A vicious cycle is thus initiated whereby sleeplessness leads to an increased perception of pain, which in turn creates needless anxiety and inhibits sleep. The importance of viewing these responses as cyclical emphasizes that the progressive care nurse may intervene anywhere in the cycle of responses and make a major impact on all three; for example, providing pain-relieving strategies that permit sleep automatically decreases anxiety. A focus on information sharing may ease the patient’s mind so that sleep can occur and pain perception decreases. The nurse has a significant role in intervening to stop this vicious cycle through a variety of holistic strategies.
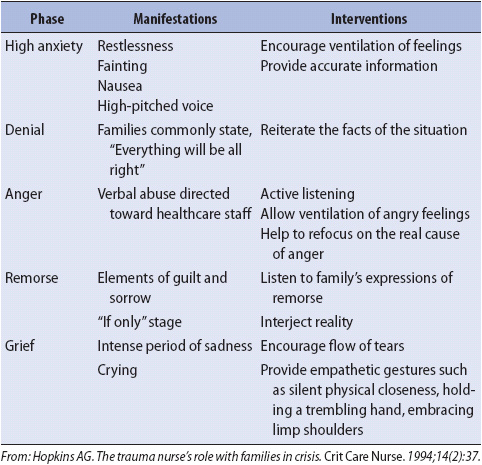
All families of trauma patients experience a crisis. Families may have no idea of how to act or what the healthcare team expects of them. Clinicians have a key role in providing the right amount of support and information to meet family needs, and in identifying family-coping mechanisms. Knowing the phases of family emotional response and suggested interventions is useful (Table 17-8). Early assessment of family system structure, relationship process, and family functioning are keys to effective management of the psychosocial needs of the patient and family. Getting to know and work with family members in trauma care is essential and can be best facilitated with flexible visiting policies, family presence during rounds, procedures, and codes when appropriate, and where family members are wanted and expected by the patient, the nurse, and the entire team.
TABLE 17-8. PHASES AND MANIFESTATIONS OF STRESS AND NURSING INTERVENTIONS FOR FAMILIES OF TRAUMA PATIENTS
AACP-SCCM Consensus Conference Committee. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101:1644-1655.
American College of Surgeons Committee on Trauma. Advanced Trauma Life Support for Doctors. 9th ed. Chicago, IL: ACS; 2012.
Aresco C. Trauma. In: Morton P, Fontaine D, eds. Critical Care Nursing: A Holistic Approach, 9th ed. New York, NY: Lippincott Williams & Wilkins; 2008.
Boswell S, Scalea T. Initial management of traumatic shock. In: McQuillan K, Makic M, Whalen E. Trauma Nursing: From Resuscitation Through Rehabilitation. 4th ed. St Louis, MO: Saunders Elsevier; 2009.
Branney SW, Wolfe RE, Moore EE, et al. Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid. J Trauma. 1995;39:375.
Cunnenn J, Cartwright M. The puzzle of sepsis: fitting the pieces of inflammatory response with treatment. AACN Clin Iss. 2004;15:18-44.
Emergency Nurses Association. Trauma Nursing Core Course-Provider Manual. 6th ed. Chicago, IL: ENA; 2007.
Feliciano DV, Mattox KL, Moore, EE. Trauma. 6th ed. New York, NY: McGraw-Hill Co; 2008.
Frawley P. Thoracic trauma. In: McQuillan K, Makic M, Whalen E, eds. Trauma Nursing: From Resuscitation Through Rehabilitation. 4th ed. St Louis, MO: Saunders Elsevier; 2009.
Goldstein AS, Scalfani SJA, Kupterstein NH, et al. The diagnostic superiority of computed tomography. J Trauma. 1985;25:939.
Jones K, Abdominal injuries. In: McQuillan K, Makic M, Whalen E, eds. Trauma Nursing: From Resuscitation Through Rehabilitation. 4th ed. St Louis, MO: Saunders Elsevier; 2009.
Levy M, Fink M, Marshall J, et al. 2001 SCCM/ESICM/ATS/SIS International sepsis definitions conference. CCM. 2003;31:1250-1256.
Mattox K, Feliciano D, Moore E, ed. Trauma. 4th ed. New York, NY: McGraw Hill; 2000.
McKinney MG, Lentz K, Nunez D, et al. Can ultrasound replace diagnostic peritoneal lavage in the assessment of blunt trauma?
J Trauma. 1994;37:439.
McQuillan K, Makic M, Whalen E. Trauma Nursing: From Resuscitation Through Rehabilitation. 4th ed. St Louis, MO: Saunders Elsevier; 2009.
Otomo Y, Henmi H, Mashiko K, et al. New diagnostic peritoneal lavage criteria for diagnosis of intestinal injury. J Trauma. 1998;44:991.
Ruggiero M. Effects of vasopressin in septic shock. AACN Advance Crit Care. 2008;19:281-290.
Rushton C, Reina M, Reina D. Building trustworthy relationships with critically ill patients and families. AACN Adv Crit Care. 2007;18:19-30.
Saunders CJ, Battistella FD, Whetzel TP, Stokes RB. Percutaneous diagnostic peritoneal lavage using a Veress needle versus an open technique: a prospective randomized trial. J Trauma. 1998;44:883.
VonRueden K, Bolton P, Vary T. Shock and multiple organ dysfunction syndrome. In: McQuillan K, Makic M, Whalen E, eds. Trauma Nursing: From Resuscitation Through Rehabilitation. 4th ed. St Louis, MO: Saunders Elsevier; 2009.
Wiegand D, Carlson K. AACN Procedure Manual for Critical Care. 5th ed. St Louis, MO: Elsevier Saunders; 2005.
http://www.aacn.org. Accessed June 29, 2013.
http://www.east.org. Accessed June 29, 2013.
http://www.trauma.org. Accessed June 29, 2013.
http://www.facs.org. Accessed June 29, 2013.
http://www.sccm.org. Accessed June 29, 2013.
http://www.ena.org. Accessed June 29, 2013.
Dellinger P, Levy MM, Carlet JM, Bion J, et al. Surviving sepsis campaign guidelines: international guidelines for management of severe sepsis and septic shock. Crit Care Med. 2008;36(1):296-327.
Geerts W, Bergqvist D, Pineo G, et al. Prevention of venous thromboembolism. Chest. 2008;133:381S-453S.