2
Common Symptoms
Paul L. Nadler, MD
Ralph Gonzales, MD, MSPH
COUGH
ESSENTIAL INQUIRIES

 Age, tobacco use, e-cigarette vaping, cannabis use, occupational history, environmental exposures, and duration of cough.
Age, tobacco use, e-cigarette vaping, cannabis use, occupational history, environmental exposures, and duration of cough.
 Dyspnea (at rest or with exertion).
Dyspnea (at rest or with exertion).
 Vital signs (heart rate, respiratory rate, body temperature).
Vital signs (heart rate, respiratory rate, body temperature).
 Chest examination.
Chest examination.
 Chest radiography when unexplained cough lasts more than 3–6 weeks.
Chest radiography when unexplained cough lasts more than 3–6 weeks.
 General Considerations
General Considerations
Cough is the most common symptom for which patients seek medical attention. Cough adversely affects personal and work-related interactions, disrupts sleep, and often causes discomfort of the throat and chest wall. Most people seeking medical attention for acute cough desire symptom relief; few are worried about serious illness. Cough results from stimulation of mechanical or chemical afferent nerve receptors in the bronchial tree. Effective cough depends on an intact afferent–efferent reflex arc, adequate expiratory and chest wall muscle strength, and normal mucociliary production and clearance.
 Clinical Findings
Clinical Findings
A. Symptoms
Distinguishing acute (less than 3 weeks), persistent (3–8 weeks), and chronic (more than 8 weeks) cough illness syndromes is a useful first step in evaluation. Postinfectious cough lasting 3–8 weeks has also been referred to as subacute cough to distinguish this common, distinct clinical entity from acute and chronic cough.
1. Acute cough—In healthy adults, most acute cough syndromes are due to viral respiratory tract infections. Additional features of infection such as fever, nasal congestion, and sore throat help confirm this diagnosis. Dyspnea (at rest or with exertion) may reflect a more serious condition, and further evaluation should include assessment of oxygenation (pulse oximetry or arterial blood gas measurement), airflow (peak flow or spirometry), and pulmonary parenchymal disease (chest radiography). The timing and character of the cough are not very useful in establishing the cause of acute cough syndromes, although cough-variant asthma should be considered in adults with prominent nocturnal cough, and persistent cough with phlegm increases the likelihood of chronic obstructive pulmonary disease (COPD). The presence of posttussive emesis or inspiratory whoop in adults modestly increases the likelihood of pertussis, and the absence of paroxysmal cough and the presence of fever decrease its likelihood. Uncommon causes of acute cough should be suspected in those with heart disease (heart failure [HF]) or hay fever (allergic rhinitis) and those with occupational risk factors (such as farmworkers).
2. Persistent and chronic cough—Cough due to acute respiratory tract infection resolves within 3 weeks in the vast majority (more than 90%) of patients. Pertussis should be considered in adolescents and adults who have persistent or severe cough lasting more than 3 weeks, who have not recently been boosted with Tdap, and who have been exposed to a person with confirmed pertussis. It should also be considered in selected geographic areas where its prevalence approaches 20% (although its exact prevalence is difficult to ascertain due to the limited sensitivity of diagnostic tests).
When angiotensin-converting enzyme (ACE) inhibitor therapy, acute respiratory tract infection, and chest radiograph abnormalities are absent, most cases of persistent and chronic cough are due to (or exacerbated by) postnasal drip (upper airway cough syndrome), asthma, or gastroesophageal reflux disease (GERD), or some combination of these three entities. Approximately 10% of cases are caused by nonasthmatic eosinophilic bronchitis. A history of nasal or sinus congestion, wheezing, or heartburn should direct subsequent evaluation and treatment, though these conditions frequently cause persistent cough in the absence of typical symptoms. Dyspnea at rest or with exertion is not commonly reported among patients with persistent cough; dyspnea requires assessment for chronic lung disease, HF, anemia, pulmonary embolism, or pulmonary hypertension.
Bronchogenic carcinoma is suspected when cough is accompanied by unexplained weight loss, hemoptysis, and fevers with night sweats, particularly in persons with significant tobacco or occupational exposures (asbestos, radon, diesel exhaust, and metals). Persistent and chronic cough accompanied by excessive mucus secretions increases the likelihood of COPD, particularly among smokers, or of bronchiectasis if accompanied by a history of recurrent or complicated pneumonia; chest radiographs are helpful in diagnosis. Chronic cough with dry eyes may represent Sjögren syndrome. A chronic dry cough may be the first symptom of idiopathic pulmonary fibrosis.
B. Physical Examination
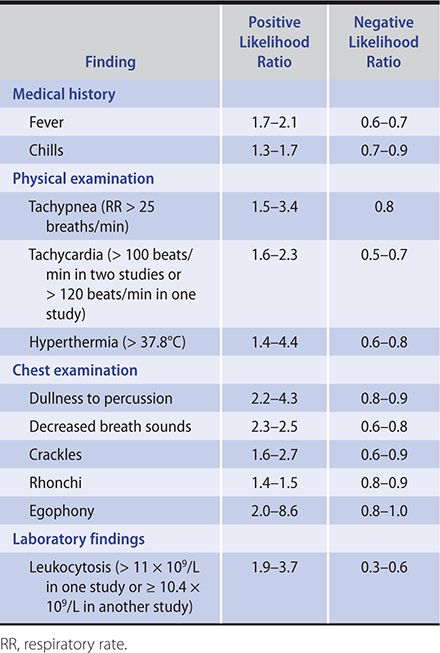
Examination can direct subsequent diagnostic testing for acute cough. Pneumonia is suspected when acute cough is accompanied by vital sign abnormalities (tachycardia, tachypnea, fever). Findings suggestive of airspace consolidation (crackles, decreased breath sounds, fremitus, egophony) are significant predictors of community-acquired pneumonia but are present in a minority of cases. Purulent sputum is associated with bacterial infections in patients with structural lung disease (eg, COPD, cystic fibrosis), but it is a poor predictor of pneumonia in the otherwise healthy adult. Wheezing and rhonchi are frequent findings in adults with acute bronchitis and do not indicate consolidation or adult-onset asthma in most cases.
Examination of patients with persistent cough should look for evidence of chronic sinusitis, contributing to postnasal drip syndrome or asthma. Chest and cardiac signs may help distinguish COPD from HF. In patients with cough and dyspnea, a normal match test (ability to blow out a match from 25 cm away) and maximum laryngeal height greater than 4 cm (measured from the sternal notch to the cricoid cartilage at end expiration) substantially decrease the likelihood of COPD. Similarly, normal jugular venous pressure and no hepatojugular reflux decrease the likelihood of biventricular HF.
C. Diagnostic Studies
1. Acute cough—Chest radiography should be considered for any adult with acute cough whose vital signs are abnormal or whose chest examination suggests pneumonia. The relationship between specific clinical findings and the probability of pneumonia is shown in Table 2–1. A large, multicenter randomized clinical trial found that elevated serum C-reactive protein (levels greater than 30 mg/dL) improves diagnostic accuracy of clinical prediction rules for pneumonia in adults with acute cough; procalcitonin added no clinically relevant information. A meta-analysis found that lung ultrasonography had better accuracy than chest radiography for the diagnosis of adult community-acquired pneumonia. Lung ultrasonography had a pooled sensitivity of 0.95 (95% confidence interval [CI], 0.93–0.97) and a specificity of 0.90 (95% CI, 0.86–0.94). Chest radiography had a pooled sensitivity of 0.77 (95% CI, 0.73–0.80) and a specificity of 0.91 (95% CI, 0.87–0.94). In patients with dyspnea, pulse oximetry and peak flow help exclude hypoxemia or obstructive airway disease. However, a normal pulse oximetry value (eg, greater than 93%) does not rule out a significant alveolar–arterial (A–a) gradient when patients have effective respiratory compensation. During documented outbreaks, clinical diagnosis of influenza has a positive predictive value of ~70%; this usually obviates the need for rapid diagnostic tests. No evidence exists to assess whether the initial evaluation of cough in immunocompromised patients should differ from immunocompetent patients, but expert recommendations suggest that tuberculosis be considered in HIV-infected patients in areas with a high prevalence of tuberculosis regardless of radiographic findings.
Table 2–1. Positive and negative likelihood ratios for history, physical examination, and laboratory findings in the diagnosis of pneumonia.
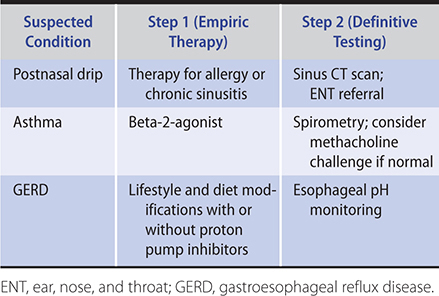
2. Persistent and chronic cough—Chest radiography is indicated when ACE inhibitor therapy–related and postinfectious cough are excluded. If pertussis is suspected, polymerase chain reaction testing should be performed on a nasopharyngeal swab or nasal wash specimen—although the ability to detect pertussis decreases as the duration of cough increases. When the chest film is normal, postnasal drip, asthma, or GERD are the most likely causes. The presence of typical symptoms of these conditions directs further evaluation or empiric therapy, though typical symptoms are often absent. Definitive tests for determining the presence of each are available (Table 2–2). However, empiric treatment with a maximum-strength regimen for postnasal drip, asthma, or GERD for 2–4 weeks is one recommended approach since documenting the presence of postnasal drip, asthma, or GERD does not mean they are the cause of the cough. Alternative approaches to identifying patients who have asthma with its corticosteroid-responsive cough include examining induced sputum for increased eosinophil counts (greater than 3%) or providing an empiric trial of prednisone, 30 mg daily orally for 2 weeks. Spirometry may help identify large airway obstruction in patients who have persistent cough and wheezing and who are not responding to asthma treatment. When empiric treatment trials are not successful, additional evaluation with pH manometry, endoscopy, barium swallow, sinus CT, or high-resolution chest CT may identify the cause.
Table 2–2. Empiric therapy or definitive testing for persistent cough.
 Differential Diagnosis
Differential Diagnosis
A. Acute Cough
Acute cough may be a symptom of acute respiratory tract infection, asthma, allergic rhinitis, HF, and ACE inhibitor therapy, as well as many less common causes.
B. Persistent and Chronic Cough
Causes of persistent cough include environmental exposures (cigarette smoke, air pollution), occupational exposures, pertussis, postnasal drip, asthma (including cough-variant asthma), GERD, COPD, chronic aspiration, bronchiectasis, eosinophilic bronchitis, tuberculosis or other chronic infection, interstitial lung disease, and bronchogenic carcinoma. COPD is a common cause of persistent cough among patients older than 50 years. Persistent cough may also be due to somatic cough syndrome (previously called “psychogenic cough”) or tic cough (previously called “habit cough”).
 Treatment
Treatment
A. Acute Cough
Treatment of acute cough should target the underlying etiology of the illness, the cough reflex itself, and any additional factors that exacerbate the cough. Cough duration is typically 1–3 weeks, yet patients frequently expect cough to last fewer than 10 days. Limited studies on the use of dextromethorphan suggest a minor or modest benefit.
When influenza is diagnosed (including H1N1 influenza), oral oseltamivir or zanamivir or intravenous peramivir are equally effective (1 less day of illness) when initiated within 30–48 hours of illness onset; treatment is recommended regardless of illness duration when patients have severe, complicated, or progressive influenza and in patients requiring hospitalization. In Chlamydophila- or Mycoplasma-documented infection or outbreaks, first-line antibiotics include erythromycin or doxycycline. Antibiotics do not improve cough severity or duration in patients with uncomplicated acute bronchitis. In patients with bronchitis and wheezing, inhaled beta-2-agonist therapy reduces severity and duration of cough. In patients with acute cough, treating the accompanying postnasal drip (with antihistamines, decongestants, saline nasal irrigation, or nasal corticosteroids) can be helpful. A Cochrane review (n = 163) found codeine to be no more effective than placebo in reducing cough symptoms.
B. Persistent and Chronic Cough
Evaluation and management of persistent cough often require multiple visits and therapeutic trials, which frequently lead to frustration, anger, and anxiety. When pertussis infection is suspected early in its course, treatment with a macrolide antibiotic (see Chapter 33) is appropriate to reduce organism shedding and transmission. When pertussis has lasted more than 7–10 days, antibiotic treatment does not affect the duration of cough, which can last up to 6 months. Early identification, revaccination with Tdap, and treatment of adult patients who work or live with persons at high risk for complications from pertussis (pregnant women, infants [particularly younger than 1 year], and immunosuppressed individuals) are encouraged.
Table 2–2 outlines empiric treatments for persistent cough. There is no evidence to guide how long to continue treatment for persistent cough due to postnasal drip, asthma, or GERD. Studies have not found a consistent benefit of inhaled corticosteroid therapy in adults with persistent cough. Eight weeks of thrice-weekly azithromycin did not improve cough in patients without asthma.
When empiric treatment trials fail, consider other causes of chronic cough such as obstructive sleep apnea, tonsillar or uvular enlargement, and environmental fungi. The small percentage of patients with idiopathic chronic cough should be managed in consultation with an otolaryngologist or a pulmonologist; consider a high-resolution CT scan of the lungs. Treatment options include nebulized lidocaine therapy and morphine sulfate, 5–10 mg orally twice daily. Sensory dysfunction of the laryngeal branches of the vagus nerve may contribute to persistent cough syndromes and may help explain the effectiveness of gabapentin in patients with chronic cough. Speech pathology therapy combined with pregabalin has some benefit in chronic refractory cough. In patients with reflex cough syndrome, therapy aimed at shifting the patient’s attentional focus from internal stimuli to external focal points can be helpful. Proton pump inhibitors are not effective on their own; most benefit appears to come from lifestyle modifications and weight reduction.
 When to Refer
When to Refer
• Failure to control persistent or chronic cough following empiric treatment trials.
• Patients with recurrent symptoms should be referred to an otolaryngologist, pulmonologist, or gastroenterologist.
 When to Admit
When to Admit
• Patient at high risk for tuberculosis for whom compliance with respiratory precautions is uncertain.
• Need for urgent bronchoscopy, such as suspected foreign body.
• Smoke or toxic fume inhalational injury.
• Gas exchanged is impaired by cough.
• Patients at high risk for barotrauma (eg, recent pneumothorax).
Hill AT et al; CHEST Expert Cough Panel. Adult outpatients with acute cough due to suspected pneumonia or influenza: CHEST Guideline and Expert Panel Report. Chest. 2019 Jan;155(1):155–67. [PMID: 30296418]
Moore A et al; CHEST Expert Cough Panel. Clinically diagnosing pertussis-associated cough in adults and children: CHEST Guideline and Expert Panel Report. Chest. 2019 Jan;155(1):147–54. [PMID: 30321509]
Sinharay R et al. Respiratory and cardiovascular responses to walking down a traffic-polluted road compared with walking in a traffic-free area in participants aged 60 years and older with chronic lung or heart disease and age-matched healthy controls: a randomised, crossover study. Lancet. 2018 Jan 27;391(10118):339–49. [PMID: 29221643]
Smith SM et al. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2017 Jun 19;6:CD000245. [PMID: 28626858]
DYSPNEA
ESSENTIAL INQUIRIES

 Fever, cough, and chest pain.
Fever, cough, and chest pain.
 Vital sign measurements; pulse oximetry.
Vital sign measurements; pulse oximetry.
 Cardiac and chest examination.
Cardiac and chest examination.
 Chest radiography and arterial blood gas measurement in selected patients.
Chest radiography and arterial blood gas measurement in selected patients.
 General Considerations
General Considerations
Dyspnea is a subjective experience or perception of uncomfortable breathing. There is a lack of empiric evidence on the prevalence, etiology, and prognosis of dyspnea in general practice. The relationship between level of dyspnea and the severity of underlying disease varies widely among individuals. Dyspnea can result from conditions that increase the mechanical effort of breathing (eg, asthma, COPD, restrictive lung disease, respiratory muscle weakness), conditions that produce compensatory tachypnea (eg, hypoxemia, acidosis), primary pulmonary vasculopathy (pulmonary hypertension), or psychogenic conditions. The following factors play a role in how and when dyspnea presents in patients: rate of onset, previous dyspnea, medications, comorbidities, psychological profile, and severity of underlying disorder.
 Clinical Findings
Clinical Findings
A. Symptoms
The duration, severity, and periodicity of dyspnea influence the tempo of the clinical evaluation. Rapid onset or severe dyspnea in the absence of other clinical features should raise concern for pneumothorax, pulmonary embolism, or increased left ventricular end-diastolic pressure (LVEDP). Spontaneous pneumothorax is usually accompanied by chest pain and occurs most often in thin, young males and in those with underlying lung disease. Pulmonary embolism should always be suspected when a patient with new dyspnea reports a recent history (previous 4 weeks) of prolonged immobilization or surgery, estrogen therapy, or other risk factors for deep venous thrombosis (DVT) (eg, previous history of thromboembolism, cancer, obesity, lower extremity trauma) and when the cause of dyspnea is not apparent. Silent myocardial infarction, which occurs more frequently in diabetic persons and women, can result in increased LVEDP, acute HF, and dyspnea.
Accompanying symptoms provide important clues to causes of dyspnea. When cough and fever are present, pulmonary disease (particularly infection) is the primary concern; myocarditis, pericarditis, and septic emboli can present in this manner. Chest pain should be further characterized as acute or chronic, pleuritic or exertional. Although acute pleuritic chest pain is the rule in acute pericarditis and pneumothorax, most patients with pleuritic chest pain in the outpatient clinic have pleurisy due to acute viral respiratory tract infection. Periodic chest pain that precedes the onset of dyspnea suggests myocardial ischemia or pulmonary embolism. When associated with wheezing, most cases of dyspnea are due to acute bronchitis; however, other causes include new-onset asthma, foreign body, and vocal cord dysfunction. Interstitial lung disease and pulmonary hypertension should be considered in patients with symptoms (or history) of connective tissue disease. Pulmonary lymphangitis carcinomatosis should be considered if a patient has a malignancy, especially breast, lung, or gastric cancer.
When a patient reports prominent dyspnea with mild or no accompanying features, consider noncardiopulmonary causes of impaired oxygen delivery (anemia, methemoglobinemia, cyanide ingestion, carbon monoxide poisoning), metabolic acidosis, panic disorder, neuromuscular disorders, and chronic pulmonary embolism.
Platypnea-orthodeoxia syndrome is characterized by dyspnea and hypoxemia on sitting or standing that improves in the recumbent position. It may be caused by an intracardiac shunt, pulmonary vascular shunt (including hepatopulmonary syndrome), or ventilation-perfusion mismatch. Hyperthyroidism can cause dyspnea from increased ventilatory drive, respiratory muscle weakness, or pulmonary hypertension.
B. Physical Examination
A focused physical examination should include evaluation of the head and neck, chest, heart, and lower extremities. Visual inspection of the patient can suggest obstructive airway disease (pursed-lip breathing, use of accessory respiratory muscles, barrel-shaped chest), pneumothorax (asymmetric excursion), or metabolic acidosis (Kussmaul respirations). Patients with impending upper airway obstruction (eg, epiglottitis, foreign body) or severe asthma exacerbation sometimes assume a tripod position. Focal wheezing raises the suspicion for a foreign body or other bronchial obstruction. Maximum laryngeal height (the distance between the top of the thyroid cartilage and the suprasternal notch at end expiration) is a measure of hyperinflation. Obstructive airway disease is virtually nonexistent when a nonsmoking patient younger than age 45 years has a maximum laryngeal height greater than 4 cm.
Factors increasing the likelihood of obstructive airway disease include patient history of more than 40 pack-years smoking (adjusted likelihood ratio [LR]+ 11.6; LR– 0.9), patient age 45 years or older (LR+ 1.4; LR– 0.5), and maximum laryngeal height greater than or equal to 4 cm (LR+ 3.6; LR– 0.7). With all three of these factors present, the LR+ rises to 58.5 and the LR– falls to 0.3.
Absent breath sounds suggest a pneumothorax. An accentuated pulmonic component of the second heart sound (loud P2) is a sign of pulmonary hypertension and pulmonary embolism.
Clinical predictors of increased LVEDP in dyspneic patients with no prior history of HF include tachycardia, systolic hypotension, jugular venous distention, hepatojugular reflux, bibasilar crackles, third heart sound, lower extremity edema, and chest film findings of pulmonary vascular redistribution or cardiomegaly. When none is present, there is a very low probability (less than 10%) of increased LVEDP, but when two or more are present, there is a very high probability (greater than 90%) of increased LVEDP.
C. Diagnostic Studies
Causes of dyspnea that can be managed without chest radiography are few: ingestions causing lactic acidosis, anemia, methemoglobinemia, and carbon monoxide poisoning. The diagnosis of pneumonia should be confirmed by chest radiography in most patients, and elevated blood levels of procalcitonin or C-reactive protein can support the diagnosis of pneumonia in equivocal cases or in the presence of interstitial lung disease. Conversely, a low procalcitonin can help exclude pneumonia in dyspneic patients presenting with HF.
Chest radiography is fairly sensitive and specific for new-onset HF (represented by redistribution of pulmonary venous circulation) and can help guide treatment of patients with other cardiac diseases. NT-proBNP can assist in the diagnosis of HF.
Lung ultrasonography is superior to chest radiography in detecting pulmonary edema due to acute decompensated HF among adult patients presenting with dyspnea and in the diagnosis of pneumonia in patients admitted to an acute geriatric ward. End-expiratory chest radiography enhances detection of small pneumothoraces.
A normal chest radiograph has substantial diagnostic value. When there is no physical examination evidence of COPD or HF and the chest radiograph is normal, the major remaining causes of dyspnea include pulmonary embolism, Pneumocystis jirovecii infection (the initial radiograph may be normal in up to 25%), upper airway obstruction, foreign body, anemia, and metabolic acidosis. If a patient has tachycardia and hypoxemia but a normal chest radiograph and electrocardiogram (ECG), then tests to exclude pulmonary emboli, anemia, or metabolic acidosis are warranted. High-resolution chest CT is particularly useful in the evaluation of interstitial and alveolar lung disease. Helical (“spiral”) CT is useful to diagnose pulmonary embolism since the images are high resolution and require only one breathhold by the patient, but to minimize unnecessary testing and radiation exposure, the clinician should first consider a clinical decision rule (with or without D-dimer testing) to estimate the pretest probability of a pulmonary embolism. It is appropriate to forego CT scanning in patients with very low probability of pulmonary embolus when other causes of dyspnea are more likely (see Chapter 9).
Laboratory findings suggesting increased LVEDP include elevated serum B-type natriuretic peptide (BNP or NT-proBNP) levels. BNP has been shown to reliably diagnose severe dyspnea caused by HF and to differentiate it from dyspnea due to other conditions.
Arterial blood gas measurement may be considered if clinical examination and routine diagnostic testing are equivocal. With two notable exceptions (carbon monoxide poisoning and cyanide toxicity), arterial blood gas measurement distinguishes increased mechanical effort causes of dyspnea (respiratory acidosis with or without hypoxemia) from compensatory tachypnea (respiratory alkalosis with or without hypoxemia or metabolic acidosis) and from psychogenic dyspnea (respiratory alkalosis). An observational study, however, found that arterial blood gas measurement had little value in determining the cause of dyspnea in patients presenting to the emergency department. Carbon monoxide and cyanide impair oxygen delivery with minimal alterations in Po2; percent carboxyhemoglobin identifies carbon monoxide toxicity. Cyanide poisoning should be considered in a patient with profound lactic acidosis following exposure to burning vinyl (such as a theater fire or industrial accident). Suspected carbon monoxide poisoning or methemoglobinemia can also be confirmed with venous carboxyhemoglobin or methemoglobin levels. Venous blood gas testing is also an option for assessing respiratory and acid-base status by measuring venous pH and Pco2 but is unable to provide information on oxygenation status. To correlate with arterial blood gas values, venous pH is typically 0.03–0.05 units lower, and venous Pco2 is typically 4–5 mm Hg higher than arterial samples.
Because arterial blood gas testing is impractical in most outpatient settings, pulse oximetry has assumed a central role in the office evaluation of dyspnea. Oxygen saturation values above 96% almost always correspond with a Po2 greater than 70 mm Hg, whereas values less than 94% may represent clinically significant hypoxemia. Important exceptions to this rule include carbon monoxide toxicity, which leads to a normal oxygen saturation (due to the similar wavelengths of oxyhemoglobin and carboxyhemoglobin), and methemoglobinemia, which results in an oxygen saturation of about 85% that fails to increase with supplemental oxygen. A delirious or obtunded patient with obstructive lung disease warrants immediate measurement of arterial blood gases to exclude hypercapnia and the need for intubation, regardless of the oxygen saturation. If a patient reports dyspnea with exertion, but resting oximetry is normal, assessment of desaturation with ambulation (eg, a brisk walk around the clinic) can be useful for confirming impaired gas exchange.
A study found that for adults without known cardiac or pulmonary disease reporting dyspnea on exertion, spirometry, NT-proBNP, and CT imaging were the most informative tests.
Episodic dyspnea can be challenging if an evaluation cannot be performed during symptoms. Life-threatening causes include recurrent pulmonary embolism, myocardial ischemia, and reactive airway disease. When associated with audible wheezing, vocal cord dysfunction should be considered, particularly in a young woman who does not respond to asthma therapy. Spirometry is very helpful in further classifying patients with obstructive airway disease but is rarely needed in the initial or emergent evaluation of patients with acute dyspnea.
 Differential Diagnosis
Differential Diagnosis
Urgent and emergent conditions causing acute dyspnea include pneumonia, COPD, asthma, pneumothorax, pulmonary embolism, cardiac disease (eg, HF, acute myocardial infarction, valvular dysfunction, arrhythmia, intracardiac shunt), pleural effusion, diffuse alveolar hemorrhage, metabolic acidosis, cyanide toxicity, methemoglobinemia, and carbon monoxide poisoning. The etiology of dyspnea secondary to e-cigarette vaping is being actively studied. Chronic dyspnea may be caused by interstitial lung disease, pulmonary hypertension, or pulmonary alveolar proteinosis.
 Treatment
Treatment
The treatment of urgent or emergent causes of dyspnea should aim to relieve the underlying cause. Pending diagnosis, patients with hypoxemia should be immediately provided supplemental oxygen unless significant hypercapnia is present or strongly suspected pending arterial blood gas measurement. Dyspnea frequently occurs in patients nearing the end of life. Opioid therapy, anxiolytics, and corticosteroids can provide substantial relief independent of the severity of hypoxemia. However, inhaled opioids are not effective. Oxygen therapy is most beneficial to patients with significant hypoxemia (Pao2 less than 55 mm Hg) (see Chapter 5). In patients with severe COPD and hypoxemia, oxygen therapy improves exercise performance and mortality. Pulmonary rehabilitation programs are another therapeutic option for patients with moderate to severe COPD or interstitial pulmonary fibrosis. Noninvasive ventilation may be considered for patients with dyspnea caused by an acute COPD exacerbation, but the efficacy of this treatment is still uncertain.
 When to Refer
When to Refer
• Following acute stabilization, patients with advanced COPD should be referred to a pulmonologist, and patients with HF or valvular heart disease should be referred to a cardiologist.
• Cyanide toxicity or carbon monoxide poisoning should be managed in conjunction with a toxicologist.
• Lung transplantation can be considered for patients with advanced interstitial lung disease.
 When to Admit
When to Admit
• Impaired gas exchange from any cause or high risk of pulmonary embolism pending definitive diagnosis.
• Suspected cyanide toxicity or carbon monoxide poisoning.
Freund Y et al; PROPER Investigator Group. Effect of the Pulmonary Embolism Rule-Out Criteria on subsequent thromboembolic events among low-risk emergency department patients: the PROPER randomized clinical trial. JAMA. 2018 Feb 13;319(6):559–66. [PMID: 29450523]
Layden JE et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin—preliminary report. N Engl J Med. 2020 Mar 5;382(10):903–16. [PMID: 31491072]
Maw AM et al. Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: a systematic review and meta-analysis. JAMA Netw Open. 2019 Mar 1;2(3):e190703. [PMID: 30874784]
Sendama W et al. Decision-making with D-dimer in the diagnosis of pulmonary embolism. Am J Med. 2018 Dec 131(12):1438–43. [PMID: 30125536]
HEMOPTYSIS
ESSENTIAL INQUIRIES

 Fever, cough, and other symptoms of lower respiratory tract infection.
Fever, cough, and other symptoms of lower respiratory tract infection.
 Smoking history.
Smoking history.
 Nasopharyngeal or gastrointestinal bleeding.
Nasopharyngeal or gastrointestinal bleeding.
 Chest radiography and complete blood count (and, in some cases, INR).
Chest radiography and complete blood count (and, in some cases, INR).
 General Considerations
General Considerations
Hemoptysis is the expectoration of blood that originates below the vocal cords. It is commonly classified as trivial, mild, or massive—the latter defined as more than 200–600 mL (about 1–2 cups) in 24 hours. Massive hemoptysis can be usefully defined as any amount that is hemodynamically significant or threatens ventilation. Its in-hospital mortality was 6.5% in one study. The initial goal of management of massive hemoptysis is therapeutic, not diagnostic.
The causes of hemoptysis can be classified anatomically. Blood may arise from the trachea due to malignant invasion, and from the airways in COPD, bronchiectasis, bronchial Dieulafoy disease, and bronchogenic carcinoma; from the pulmonary vasculature in left ventricular failure, mitral stenosis, pulmonary embolism, pulmonary arterial hypertension, and arteriovenous malformations; or from the pulmonary parenchyma in pneumonia, fungal infections, inhalation of crack cocaine, or granulomatosis with polyangiitis. Diffuse alveolar hemorrhage—manifested by alveolar infiltrates on chest radiography—is due to small vessel bleeding usually caused by autoimmune or hematologic disorders, or rarely precipitated by warfarin. Most cases of hemoptysis presenting in the outpatient setting are due to infection (eg, acute or chronic bronchitis, pneumonia, tuberculosis, aspergillosis). Hemoptysis due to lung cancer increases with age, causing up to 20% of cases among older adults. Less commonly (less than 10% of cases), pulmonary venous hypertension (eg, mitral stenosis, pulmonary embolism) causes hemoptysis. Most cases of hemoptysis that have no visible cause on CT scan or bronchoscopy will resolve within 6 months without treatment, with the notable exception of patients at high risk for lung cancer (smokers older than 40 years). Iatrogenic hemorrhage may follow transbronchial lung biopsies, anticoagulation, or pulmonary artery rupture due to distal placement of a balloon-tipped catheter. Obstructive sleep apnea may be a risk factor for hemoptysis. Amyloidosis of the lung can cause hemoptysis. No cause is identified in up to 15–30% of cases.
 Clinical Findings
Clinical Findings
A. Symptoms
Blood-tinged sputum in the setting of an upper respiratory tract infection in an otherwise healthy, young (age under 40 years) nonsmoker does not warrant an extensive diagnostic evaluation if the hemoptysis subsides with resolution of the infection. However, hemoptysis is frequently a sign of serious disease, especially in patients with a high prior probability of underlying pulmonary pathology. Hemoptysis is the only symptom found to be a specific predictor of lung cancer. There is no value in distinguishing blood-streaked sputum and cough productive of blood during evaluation; the goal of the history is to identify patients at risk for one of the disorders listed earlier. Pertinent features include duration of symptoms, presence of respiratory infection, and past or current tobacco use. Nonpulmonary sources of hemorrhage—from the sinuses or the gastrointestinal tract—must be excluded.
B. Physical Examination
Elevated pulse, hypotension, and decreased oxygen saturation suggest large-volume hemorrhage that warrants emergent evaluation and stabilization. The nares and oropharynx should be carefully inspected to identify a potential upper airway source of bleeding. Chest and cardiac examination may reveal evidence of HF or mitral stenosis.
C. Diagnostic Studies
Diagnostic evaluation should include a chest radiograph and complete blood count. Kidney function tests, urinalysis, and coagulation studies are appropriate in specific circumstances. Hematuria that accompanies hemoptysis may be a clue to Goodpasture syndrome or vasculitis. Flexible bronchoscopy reveals endobronchial cancer in 3–6% of patients with hemoptysis who have a normal (non-lateralizing) chest radiograph. Nearly all of these patients are smokers over the age of 40, and most will have had symptoms for more than 1 week. High-resolution chest CT scan complements bronchoscopy; it can visualize unsuspected bronchiectasis and arteriovenous malformations and will show central endobronchial cancers in many cases. It is the test of choice for suspected small peripheral malignancies. Helical CT pulmonary angiography is the initial test of choice for evaluating patients with suspected pulmonary embolism, although caution should be taken to avoid large contrast loads in patients with even mild chronic kidney disease (serum creatinine greater than 2.0 g/dL or rapidly rising creatinine in normal range). Helical CT scanning can be avoided in patients who are at “unlikely” risk for pulmonary embolism using the Wells score or PERC rule for pulmonary embolism and the sensitive D-dimer test. Echocardiography may reveal evidence of HF or mitral stenosis.
 Treatment
Treatment
Management of mild hemoptysis consists of identifying and treating the specific cause. Massive hemoptysis is life-threatening. The airway should be protected with endotracheal intubation, ventilation ensured, and effective circulation maintained. If the location of the bleeding site is known, the patient should be placed in the decubitus position with the involved lung dependent. Uncontrollable hemorrhage warrants rigid bronchoscopy and surgical consultation. In stable patients, flexible bronchoscopy may localize the site of bleeding, and angiography can embolize the involved bronchial arteries. Embolization is effective initially in 85% of cases, although rebleeding may occur in up to 20% of patients during the following year. The anterior spinal artery arises from the bronchial artery in up to 5% of people, and paraplegia may result if it is inadvertently cannulated and embolized.
One double-blind, randomized controlled trial compared treatment with inhalations of tranexamic acid (an antifibrinolytic drug) versus placebo (normal saline) in patients hospitalized with mild hemoptysis (less than 200 mL of expectorated blood per 24 hours). Compared to patients receiving placebo (normal saline), more patients treated with tranexamic acid experienced resolution of hemoptysis within 5 days of admission (96% versus 50%; P < 0.0005). In addition, mean hospital length of stay was shorter for the tranexamic acid group and fewer patients required invasive procedures (interventional bronchoscopy, angiographic embolization) to control the hemorrhage.
 When to Refer
When to Refer
• Patients should be referred to a pulmonologist when bronchoscopy of the lower respiratory tract is needed.
• Patients should be referred to an otolaryngologist when an upper respiratory tract bleeding source is identified.
• Patients with severe coagulopathy complicating management should be referred to a hematologist.
 When to Admit
When to Admit
• To stabilize bleeding process in patients at risk for or experiencing massive hemoptysis.
• To correct disordered coagulation (using clotting factors or platelets, or both) or to reverse anticoagulation.
• To stabilize gas exchange.
Davidson K et al. Managing massive hemoptysis. Chest. 2020 Jan;157(1):77–88. [PMID: 31374211]
Ittrich H et al. The diagnosis and treatment of hemoptysis. Dtsch Arztebl Int. 2017 Jun 5;114(21):371–81. [PMID: 28625277]
Nasser M et al. Alveolar hemorrhage in vasculitis (primary and secondary). Semin Respir Crit Care Med. 2018 Aug;39(4):482–93. [PMID: 30404115]
Wand O et al. Inhaled tranexamic acid for hemoptysis treatment: a randomized controlled trial. Chest. 2018 Dec;154(6):1379–84. [PMID: 30321510]
CHEST PAIN
ESSENTIAL INQUIRIES

 Pain onset, character, location/size, duration, periodicity, and exacerbators; shortness of breath.
Pain onset, character, location/size, duration, periodicity, and exacerbators; shortness of breath.
 Vital signs; chest and cardiac examinations.
Vital signs; chest and cardiac examinations.
 Electrocardiography and biomarkers of myocardial necrosis in selected patients.
Electrocardiography and biomarkers of myocardial necrosis in selected patients.
 General Considerations
General Considerations
Chest pain (or chest discomfort) is a common symptom that can occur as a result of cardiovascular, pulmonary, pleural, or musculoskeletal disease; esophageal or other gastrointestinal disorders; herpes zoster; cocaine use; or anxiety states. The frequency and distribution of life-threatening causes of chest pain, such as acute coronary syndrome (ACS), pericarditis, aortic dissection, vasospastic angina, pulmonary embolism, pneumonia, and esophageal perforation, vary substantially between clinical settings. Systemic lupus erythematosus, rheumatoid arthritis, reduced estimated glomerular filtration rate, and HIV infection are conditions that confer a strong risk of coronary artery disease. Precocious ACS may represent acute thrombosis independent of underlying atherosclerotic disease. In patients aged 35 years or younger, risk factors for ACS are obesity, hyperlipidemia, and smoking.
Chest pain characteristics that can lead to early diagnosis of acute myocardial infarction do not differ in frequency or strength of association between men and women. Because pulmonary embolism can present with a wide variety of symptoms, consideration of the diagnosis and rigorous risk factor assessment for venous thromboembolism (VTE) is critical. Classic VTE risk factors include cancer, trauma, recent surgery, prolonged immobilization, pregnancy, oral contraceptives, and family history and prior history of VTE. Other conditions associated with increased risk of pulmonary embolism include HF and COPD. Sickle cell anemia can cause acute chest syndrome. Patients with this syndrome often have chest pain, fever, and cough.
 Clinical Findings
Clinical Findings
A. Symptoms
Myocardial ischemia is usually described as a dull, aching sensation of “pressure,” “tightness,” “squeezing,” or “gas,” rather than as sharp or spasmodic. Ischemic symptoms usually subside within 5–20 minutes but may last longer. Progressive symptoms or symptoms at rest may represent unstable angina. Prolonged chest pain episodes might represent myocardial infarction, although up to one-third of patients with acute myocardial infarction do not report chest pain. When present, pain due to myocardial ischemia is commonly accompanied by a sense of anxiety or uneasiness. The location is usually retrosternal or left precordial. Because the heart lacks somatic innervation, precise localization of pain due to cardiac ischemia is difficult; the pain is commonly referred to the throat, lower jaw, shoulders, inner arms, upper abdomen, or back. Ischemic pain may be precipitated or exacerbated by exertion, cold temperature, meals, stress, or combinations of these factors and is usually relieved by rest. However, many episodes do not conform to these patterns, and atypical presentations of ACS are more common in older adults, women, and persons with diabetes mellitus. Other symptoms that are associated with ACS include shortness of breath; dizziness; a feeling of impending doom; and vagal symptoms, such as nausea and diaphoresis. In older persons, fatigue is a common presenting complaint of ACS.
There are gender differences in the perception and presenting symptoms of young patients with myocardial infarction. Women were more likely than men to present with three or more associated symptoms (eg, epigastric symptoms, palpitations, and pain or discomfort in the jaw, neck, arms, or between the shoulder blades; 61.9% for women versus 54.8% for men, P < 0.001). In adjusted analyses, women with an ST-segment-elevation acute myocardial infarction were more likely than men to present without chest pain (odds ratio, 1.51; 95% CI, 1.03–2.22). In comparison with men, women were more likely to perceive symptoms as stress/anxiety (20.9% versus 11.8%, P < 0.001) but less likely to attribute symptoms to muscle pain (15.4% versus 21.2%, P = 0.03.)
One analysis found the following clinical features to be associated with acute myocardial infarction: (1) from the history: chest pain that radiates to the left, right, or both arms (LR+ 2.3, 2.9, 7.1); diaphoresis (LR+ 2.0); and nausea and vomiting (LR+1.9); (2) from the physical examination: third heart sound (LR+ 3.2), systolic blood pressure less than or equal to 80 mm Hg (LR +3.1), pulmonary crackles (LR+ 2.1); and (3) from the electrocardiogram: any ST-segment elevation greater than or equal to 1 mm (LR+ 11.2), any ST depression (LR 3.2), any Q wave (LR+ 3.9), any conduction defect (LR+ 2.7), and new conduction defect (LR+ 6.3).
A meta-analysis found the clinical findings and risk factors most suggestive of ACS were prior abnormal stress test (specificity, 96%; LR, 3.1 [95% CI, 2.0–4.7]), peripheral arterial disease (specificity, 97%; LR, 2.7 [95% CI, 1.5–4.8]), and pain radiation to both arms (specificity, 96%; LR, 2.6 [95% CI, 1.8–3.7]). The ECG findings associated with ACS were ST-segment depression (specificity, 95%; LR, 5.3 [95% CI, 2.1–8.6]) and any evidence of ischemia (specificity, 91%; LR, 3.6 [95% CI, 1.6–5.7]). Risk scores derived from both the History, Electrocardiogram, Age, Risk Factors, Troponin (HEART) and Thrombolysis in Myocardial Infarction (TIMI) trials performed well in detecting ACS (LR, 13 [95% CI, 7.0–24] for HEART score of 7–10, and LR, 6.8 [95% CI, 5.2–8.9] for TIMI score of 5–7).
Hypertrophy of either ventricle or aortic stenosis may also give rise to chest pain with less typical features. Pericarditis produces pain that may be greater when supine than upright and increases with respiration, coughing, or swallowing. Pleuritic chest pain is usually not ischemic, and pain on palpation may indicate a musculoskeletal cause. Aortic dissection classically produces an abrupt onset of tearing pain of great intensity that often radiates to the back; however, this classic presentation occurs in a small proportion of cases. Anterior aortic dissection can also lead to myocardial or cerebrovascular ischemia.
Pulmonary embolism has a wide range of clinical presentations, with chest pain present in about 75% of cases. The chief objective in evaluating patients with suspected pulmonary embolism is to assess the patient’s clinical risk for VTE based on medical history and associated symptoms and signs (see above and Chapter 9). Rupture of the thoracic esophagus iatrogenically or secondary to vomiting is another cause of chest pain.
B. Physical Examination
Findings on physical examination can occasionally yield important clues to the underlying cause of chest pain; however, a normal physical examination should never be used as the sole basis for ruling out most diagnoses, particularly ACS and aortic dissection. Vital signs (including pulse oximetry) and cardiopulmonary examination are always the first steps for assessing the urgency and tempo of the subsequent examination and diagnostic workup.
Although chest pain that is reproducible or worsened with palpation strongly suggests a musculoskeletal cause, up to 15% of patients with ACS will have reproducible chest wall tenderness. Pointing to the location of the pain with one finger has been shown to be highly correlated with nonischemic chest pain. Aortic dissection can result in differential blood pressures (greater than 20 mm Hg), pulse amplitude deficits, and new diastolic murmurs. Although hypertension is considered the rule in patients with aortic dissection, systolic blood pressure less than 100 mm Hg is present in up to 25% of patients.
A cardiac friction rub represents pericarditis until proven otherwise. It can best be heard with the patient sitting forward at end-expiration. Tamponade should be excluded in all patients with a clinical diagnosis of pericarditis by assessing pulsus paradoxus (a decrease in systolic blood pressure during inspiration greater than 10 mm Hg) and inspection of jugular venous pulsations. Subcutaneous emphysema is common following cervical esophageal perforation but present in only about one-third of thoracic perforations (ie, those most commonly presenting with chest pain).
The absence of abnormal physical examination findings in patients with suspected pulmonary embolism usually serves to increase the likelihood of pulmonary embolism, although a normal physical examination is also compatible with the much more common conditions of panic/anxiety disorder and musculoskeletal disease.
C. Diagnostic Studies
Unless a competing diagnosis can be confirmed, an ECG is warranted in the initial evaluation of most patients with acute chest pain to help exclude ACS. ST-segment elevation is the ECG finding that is the strongest predictor of acute myocardial infarction; however, up to 20% of patients with ACS can have a normal ECG. In the emergency department, patients with suspected ACS can be safely removed from cardiac monitoring if they are pain-free at initial physician assessment and have a normal or nonspecific ECG. This decision rule had 100% sensitivity for serious arrhythmia (95% CI, 80–100%). Clinically stable patients with cardiovascular disease risk factors, normal ECG, normal cardiac biomarkers, and no alternative diagnoses (such as typical GERD or costochondritis) should be followed up with a timely exercise stress test that includes perfusion imaging. However, more than 25% of patients with stable chest pain referred for noninvasive testing will have normal coronary arteries and no long-term clinical events. The ECG can also provide evidence for alternative diagnoses, such as pericarditis and pulmonary embolism. Chest radiography is often useful in the evaluation of chest pain, and is always indicated when cough or shortness of breath accompanies chest pain. Findings of pneumomediastinum or new pleural effusion are consistent with esophageal perforation. Stress echocardiography is useful in risk stratifying patients with chest pain, even among those with significant obesity.
Diagnostic protocols using a single high-sensitivity troponin assay combined with a standardized clinical assessment are an efficient strategy to rapidly determine whether patients with chest pain are at low risk and may be discharged from the emergency department. Six established risk scores are (1) the modified Goldman Risk Score, (2) TIMI Risk Score, (3) Global Registry of Acute Cardiac Events (GRACE) Risk Score, (4) HEART Risk Score, (5) Vancouver Chest Pain Rule, and (6) the European Society of Cardiology (ESC) 0/1-h algorithm. A study comparing these risk scores (not including the ESC algorithm) for predicting acute myocardial infarction within 30 days reported a sensitivity of 98% (which correlates with a negative predictive value of greater than or equal to 99.5%). Patients eligible for discharge (about 30%) were those with a TIMI score of less than or equal to 1, modified Goldman score of less than or equal to 1 with normal high-sensitivity troponin T, TIMI score of 0, or HEART score of less than or equal to 3 with normal high-sensitivity troponin I. In African-American patients with average cardiovascular risk, HEART score is a better predictive tool for 6-week major adverse cardiac events (MACE) when compared to TIMI score. Six-week MACE among patients with low-to-moderate risk based on HEART score was 3.11 (95% CI, 1.43–6.76; P = 0.004).
While some studies of high-sensitivity cardiac troponin suggest that it may be the best cardiac biomarker, it may not outperform conventional troponin assays if an appropriate cutoff is used.
Patients who arrive at the emergency department with chest pain of intermediate or high probability for ACS without electrocardiographic or biomarker evidence of a myocardial infarction can be safely discharged from an observation unit after stress cardiac MRI. Sixty-four–slice CT coronary angiography (CTA) is an alternative to stress testing in the emergency department for detecting ACS among patients with normal or nonspecific ECG and normal biomarkers. A meta-analysis of nine studies found ACS in 10% of patients, and an estimated sensitivity of CTA for ACS of 95% and specificity of 87%, yielding a negative LR of 0.06 and a positive LR of 7.4. Coronary CTA applied early in the evaluation of suspected ACS does not identify more patients with significant coronary artery disease requiring coronary revascularization, shorten hospital stay, or allow for more direct discharge from the emergency department compared to high-sensitivity troponins. Thus, functional testing appears to be the best initial noninvasive test in symptomatic patients with suspected coronary artery disease. CTA is an option for patients who do not have access to functional testing.
For patients at low risk for ACS, an initial diagnostic strategy of stress echocardiography or cardiovascular magnetic resonance is associated with similar cardiac event rates, but a substantially lower invasive testing rate.
A minimal-risk model developed by the PROMISE investigators includes 10 clinical variables that correlate with normal coronary CTA results and no clinical events (C statistic = 0.725 for the derivation and validation subsets; 95% CI, 0.705–0.746). These variables include (1) younger age; (2) female sex; (3) racial or ethnic minority; (4–6) no history of hypertension, diabetes, or dyslipidemia; (7) no family history of premature coronary artery disease; (8) never smoking; (9) symptoms unrelated to physical or mental stress; and (10) higher high-density lipoprotein cholesterol level. In the PROMISE trial, women had higher rates of normal noninvasive testing compared with men, but women with abnormalities on such testing were less likely to be referred for catheterization or to receive statin therapy.
In the evaluation of pulmonary embolism, diagnostic test decisions and results must be interpreted in the context of the clinical likelihood of VTE. A negative D-dimer test is helpful for excluding pulmonary embolism in patients with low clinical probability of VTE (3-month incidence = 0.5%); however, the 3-month risk of VTE among patients with intermediate and high risk of VTE is sufficiently high in the setting of a negative D-dimer test (3.5% and 21.4%, respectively) to warrant further imaging given the life-threatening nature of this condition if left untreated. CTA (with helical or multidetector CT imaging) has replaced ventilation-perfusion scanning as the preferred initial diagnostic test, having approximately 90–95% sensitivity and 95% specificity for detecting pulmonary embolism (compared with pulmonary angiography). However, for patients with high clinical probability of VTE, lower extremity ultrasound or pulmonary angiogram may be indicated even with a normal helical CT.
Panic disorder is a common cause of chest pain, accounting for up to 25% of cases that present to emergency departments and a higher proportion of cases presenting in primary care office practices. Features that correlate with an increased likelihood of panic disorder include absence of coronary artery disease, atypical quality of chest pain, female sex, younger age, and a high level of self-reported anxiety. Depression is associated with recurrent chest pain with or without coronary artery disease (odds ratio [OR], 2.11; 95% CI, 1.18–3.79).
 Treatment
Treatment
Treatment of chest pain should be guided by the underlying etiology. The term “noncardiac chest pain” is used when a diagnosis remains elusive after patients have undergone an extensive workup. Almost half reported symptom improvement with high-dose proton-pump inhibitor therapy. Relief of constipation may be therapeutic in proton pump inhibitor refractory noncardiac chest pain. A meta-analysis of 15 trials suggested modest to moderate benefit for psychological (especially cognitive-behavioral) interventions. It is unclear whether tricyclic or selective serotonin reuptake inhibitor antidepressants have benefit in noncardiac chest pain. Hypnotherapy may offer some benefit.
 When to Refer
When to Refer
• Refer patients with poorly controlled, noncardiac chest pain to a pain specialist.
• Refer patients with sickle cell anemia to a hematologist.
 When to Admit
When to Admit
• Failure to adequately exclude life-threatening causes of chest pain, particularly myocardial infarction, dissecting aortic aneurysm, pulmonary embolism, and esophageal rupture.
• High risk of pulmonary embolism and a positive sensitive D-dimer test.
• TIMI score of 1 or more, HEART score greater than 3, abnormal ECG, and abnormal 0- and 2-hour troponin tests.
• Pain control for rib fracture that impairs gas exchange.
Bhattacharya PT et al. Predictive risk stratification using HEART (history, electrocardiogram, age, risk factors, and initial troponin) and TIMI (thrombolysis in myocardial infarction) scores in non–high-risk chest pain patients: an African American urban community-based hospital study. Medicine (Baltimore). 2019 Aug;98(32):e16370. [PMID: 31393346]
Januzzi JL Jr et al; PROMISE Investigators. Single-molecule hsTnI and short-term risk in stable patients with chest pain. J Am Coll Cardiol. 2019 Jan 29;73(3):251–60. [PMID: 30678753]
McCarthy CP et al. Myocardial injury in the era of high-sensitivity cardiac troponin assays: a practical approach for clinicians. JAMA Cardiol. 2019 Aug 7. [Epub ahead of print] [PMID: 31389986]
Pagidipati NJ et al; PROMISE Investigators. Sex differences in management and outcomes of patients with stable symptoms suggestive of coronary artery disease: insights from the PROMISE trial. Am Heart J. 2019 Feb;208:28–36. [PMID: 30529930]
Yang S et al. The role of coronary CT angiography for acute chest pain in the era of high-sensitivity troponins. J Cardiovasc Comput Tomogr. 2019 Sep–Oct;13(5):267–273. [PMID: 31235403]
PALPITATIONS
ESSENTIAL INQUIRIES

 Forceful, rapid, or irregular beating of the heart.
Forceful, rapid, or irregular beating of the heart.
 Rate, duration, and degree of regularity of heartbeat; age at first episode.
Rate, duration, and degree of regularity of heartbeat; age at first episode.
 Factors that precipitate or terminate episodes.
Factors that precipitate or terminate episodes.
 Light-headedness or syncope; neck pounding.
Light-headedness or syncope; neck pounding.
 Chest pain; history of myocardial infarction or structural heart disease.
Chest pain; history of myocardial infarction or structural heart disease.
 General Considerations
General Considerations
Palpitations are defined as an unpleasant awareness of the forceful, rapid, or irregular beating of the heart. They are the primary symptom for approximately 16% of patients presenting to an outpatient clinic with a cardiac complaint. In an observational cohort study of palpitations at an outpatient cardiac unit, cardiac arrhythmias were the cause of palpitations in 81% of cases. Palpitations represent 5.8 of every 1000 emergency department visits, with an admission rate of 24.6%. While palpitations are usually benign, they are occasionally the symptom of a life-threatening arrhythmia. To avoid missing a dangerous cause of the patient’s symptom, clinicians sometimes pursue expensive and invasive testing when a conservative diagnostic evaluation is often sufficient. The converse is also true; in one study, 54% of patients with supraventricular tachycardia were initially wrongly diagnosed with panic, stress, or anxiety disorder. A disproportionate number of these misdiagnosed patients are women. Table 2–3 lists history, physical examination, and ECG findings suggesting a cardiovascular cause for the palpitations.
Table 2–3. Palpitations: Patients at high risk for a cardiovascular cause.
Historical risk factors
Family history of significant arrhythmias
Personal or family history of syncope or resuscitated sudden death
History of myocardial infarction (and likely scarred myocardium)
Palpitations that occur during sleep
Anatomic abnormalities
Structural heart disease such as dilated or hypertrophic cardiomyopathies
Valvular disease (stenotic or regurgitant)
ECG findings
Long QT syndrome
Bradycardia
Second- or third-degree heart block
Sustained ventricular arrhythmias
 Clinical Findings
Clinical Findings
A. Symptoms
Although described by patients in a myriad of ways, guiding the patient through a careful description of their palpitations may indicate a mechanism and narrow the differential diagnosis. Pertinent questions include the age at first episode; precipitants; and rate, duration, and degree of regularity of the heartbeat during the subjective palpitations. Palpitations lasting less than 5 minutes and a family history of panic disorder reduce the likelihood of an arrhythmic cause (LR = 0.38 and LR = 0.26, respectively). To better understand the symptom, the examiner can ask the patient to “tap out” the rhythm with his or her fingers. The circumstances associated with onset and termination can also be helpful in determining the cause. Palpitations that start and stop abruptly suggest supraventricular or ventricular tachycardias. Termination of palpitations using vagal maneuvers (eg, Valsalva maneuver) suggests supraventricular tachycardia.
Three common descriptions of palpitations are (1) “flip-flopping” (or “stop and start”), often caused by premature contraction of the atrium or ventricle, with the perceived “stop” from the pause following the contraction, and the “start” from the subsequent forceful contraction; (2) rapid “fluttering in the chest,” with regular “fluttering” suggesting supraventricular or ventricular arrhythmias (including sinus tachycardia) and irregular “fluttering” suggesting atrial fibrillation, atrial flutter, or tachycardia with variable block; and (3) “pounding in the neck” or neck pulsations, often due to “cannon” A waves in the jugular venous pulsations that occur when the right atrium contracts against a closed tricuspid valve.
Palpitations associated with chest pain suggest ischemic heart disease, or if the chest pain is relieved by leaning forward, pericardial disease. Palpitations associated with light-headedness, presyncope, or syncope suggest hypotension and may signify a life-threatening cardiac arrhythmia. Palpitations that occur regularly with exertion suggest a rate-dependent bypass tract or hypertrophic cardiomyopathy. If a benign etiology for these concerning symptoms cannot be ascertained at the initial visit, then ambulatory monitoring or prolonged cardiac monitoring in the hospital might be warranted.
Noncardiac symptoms should also be elicited since the palpitations may be caused by a normal heart responding to a metabolic or inflammatory condition. Weight loss suggests hyperthyroidism. Palpitations can be precipitated by vomiting or diarrhea that leads to electrolyte disorders and hypovolemia. Hyperventilation, hand tingling, and nervousness are common when anxiety or panic disorder is the cause of the palpitations. Palpitations associated with flushing, episodic hypertension, headaches, anxiety, and diaphoresis may be caused by a pheochromocytoma or paraganglioma. In patients with suspected pheochromocytoma or paraganglioma, a 24-hour urine collection for fractionated plasma or urinary metanephrines and catecholamines has a sensitivity and specificity of 98%.
A family history of palpitations or sudden death suggests an inherited etiology such as long QT syndrome or Brugada syndrome. Chagas disease may cause palpitations and acute myocarditis. Younger patients should be asked about consumption of “energy drinks.” Finally, dual use of cigarettes and e-cigarettes may cause palpitations.
B. Physical Examination
Rarely does the clinician have the opportunity to examine a patient during an episode of palpitations. However, careful cardiovascular examination can find abnormalities that can increase the likelihood of specific cardiac arrhythmias. The midsystolic click of mitral valve prolapse can suggest the diagnosis of a supraventricular arrhythmia. The harsh holosystolic murmur of hypertrophic cardiomyopathy, which occurs along the left sternal border and increases with the Valsalva maneuver, suggests atrial fibrillation or ventricular tachycardia. A crescendo mid-diastolic murmur may be caused by an atrial myxoma. The presence of dilated cardiomyopathy, suggested on examination by a displaced and enlarged cardiac point-of-maximal impulse, increases the likelihood of ventricular tachycardia and atrial fibrillation. In patients with chronic atrial fibrillation, in-office exercise (eg, a brisk walk in the hallway) may reveal an intermittent accelerated ventricular response as the cause of the palpitations. The clinician should also look for signs of hyperthyroidism (eg, tremulousness, brisk deep tendon reflexes, or fine hand tremor), or signs of stimulant drug use (eg, dilated pupils or skin or nasal septal perforations). Visible neck pulsations (LR, 2.68; 95% CI, 1.25–5.78) in association with palpitations increases the likelihood of atrioventricular nodal reentry tachycardia.
C. Diagnostic Studies
1. ECG—A 12-lead ECG should be performed on all patients reporting palpitations because it can provide evidence for a wide variety of causes. Although in most instances a specific arrhythmia will not be detected on the tracing, a careful evaluation of the ECG can help the clinician deduce a likely etiology in certain circumstances.
For instance, bradyarrhythmias and heart block can be associated with ventricular ectopy or escape beats that may be experienced as palpitations by the patient. Evidence of prior myocardial infarction on ECG (eg, Q waves) increases the patient’s risk for nonsustained or sustained ventricular tachycardia. Ventricular preexcitation (Wolff-Parkinson-White syndrome) is suggested by a short PR interval (less than 0.20 ms) and delta waves (upsloping PR segments). Left ventricular hypertrophy with deep septal Q waves in I, AVL, and V4 through V6 is seen in patients with hypertrophic obstructive cardiomyopathy. The presence of left atrial enlargement as suggested by a terminal P-wave force in V1 more negative than 0.04 msec and notching in lead II reflects a patient at increased risk for atrial fibrillation. A prolonged QT interval and abnormal T-wave morphology suggest the long QT syndrome, which puts patients at increased risk for ventricular tachycardia. Persistent ST-segment elevations in ECG leads V1–V3 (particularly with a coved or saddle-back pattern) suggest Brugada syndrome.
2. Monitoring devices—For high-risk patients (Table 2–3), further diagnostic studies are warranted. A step-wise approach has been suggested—starting with ambulatory monitoring devices (ambulatory ECG [Holter] monitoring if the palpitations are expected to occur within the subsequent 72-hour period, event monitoring if less frequent). An implantable loop recorder can be used for extended monitoring if clinical suspicion is high, especially if there is syncope. A single-lead, lightweight, continuously recording ambulatory adhesive patch monitor (Zio Patch) worn for 14 days has been shown to be superior to 24-hour ambulatory ECG (Holter) monitoring. This is then followed by inpatient continuous monitoring if serious arrhythmias are strongly suspected despite normal findings on the ambulatory monitoring, and by invasive electrophysiologic testing if the ambulatory or inpatient monitor records a worrisome arrhythmia. Validation studies are underway on the use of smartphone-based event recorders.
In patients with a prior myocardial infarction, ambulatory cardiac monitoring or signal-averaged ECG is an appropriate next step to help exclude ventricular tachycardia. ECG exercise testing is appropriate in patients with suspected coronary artery disease and in patients who have palpitations with physical exertion. Echocardiography is useful when physical examination or ECG suggests structural abnormalities or decreased ventricular function.
 Differential Diagnosis
Differential Diagnosis
When assessing a patient with palpitations in an urgent care setting, the clinician must ascertain whether the symptoms represent (1) an arrhythmia that is minor and transient, (2) a significant cardiovascular disease, (3) a cardiac manifestation of a systemic disease such as thyrotoxicosis, or (4) a benign somatic symptom that is amplified by the patient’s underlying psychological state.
Patients with palpitations who seek medical attention in an emergency department instead of a medical clinic are more likely to have a cardiac cause (47% versus 21%), whereas psychiatric causes are more common among those who seek attention in office practices (45% versus 27%). In a study of patients who went to a university medical clinic with the chief complaint of palpitations, causes were cardiac in 43%, psychiatric in 31%, and miscellaneous in 10%.
Cardiac arrhythmias that can result in symptoms of palpitations include sinus bradycardia; sinus, supraventricular, and ventricular tachycardia; premature ventricular and atrial contractions; sick sinus syndrome; and advanced atrioventricular block.
Cardiac nonarrhythmic causes of palpitations include valvular heart diseases, such as aortic regurgitation or stenosis, atrial or ventricular septal defect, cardiomyopathy, congenital heart disease, pericarditis, arrhythmogenic right ventricular cardiomyopathy, and atrial myxoma. Mitral valve prolapse is not associated with arrhythmic events, but ventricular arrhythmias are frequent in mitral annulus disjunction.
The most common psychiatric causes of palpitations are anxiety and panic disorder. The release of catecholamines during a significant stress or panic attack can trigger an arrhythmia. Asking a single question, “Have you experienced brief periods, for seconds or minutes, of an overwhelming panic or terror that was accompanied by racing heartbeats, shortness of breath, or dizziness?” can help identify patients with panic disorder.
Miscellaneous causes of palpitations include fever, dehydration, hypoglycemia, anemia, thyrotoxicosis, mastocytosis, and pheochromocytoma. Drugs such as cocaine, alcohol, caffeine, pseudoephedrine, and illicit ephedra can precipitate palpitations, as can prescription medications, including digoxin, amitriptyline, erythromycin and other drugs that prolong the QT interval, class 1 antiarrhythmics, dihydropyridine calcium channel blockers, phenothiazines, theophylline, and beta-agonists.
 Treatment
Treatment
After ambulatory monitoring, most patients with palpitations are found to have benign atrial or ventricular ectopy or nonsustained ventricular tachycardia. In patients with structurally normal hearts, these arrhythmias are not associated with adverse outcomes. Abstention from caffeine and tobacco may help. Often, reassurance suffices. If not, or in very symptomatic patients, a trial of a beta-blocker may be prescribed. A three-session course of cognitive-behavioral therapy that includes some physical activity has proven effective for patients with benign palpitations with or without chest pain. For treatment of specific atrial or ventricular arrhythmias, see Chapter 10.
 When to Refer
When to Refer
• For electrophysiologic studies.
• For advice regarding treatment of atrial or ventricular arrhythmias.
 When to Admit
When to Admit
• Palpitations associated with syncope or near-syncope, particularly when the patient is aged 75 years or older and has an abnormal ECG, hematocrit less than 30%, shortness of breath, respiratory rate higher than 24/min, or a history of HF.
• Patients with risk factors for a serious arrhythmia.
Clementy N et al. Benefits of an early management of palpitations. Medicine (Baltimore). 2018 Jul;97(28):e11466. [PMID: 29995805]
Giada F et al. Clinical approach to patients with palpitations. Card Electrophysiol Clin. 2018 Jun;10(2):387–96. [PMID: 29784490]
Lewalter T et al; INSIGHT XT Study Investigators. “First-degree AV block—a benign entity?” Insertable cardiac monitor in patients with 1st-degree AV block reveals presence or progression to higher grade block or bradycardia requiring pacemaker implant. J Interv Card Electrophysiol. 2018 Aug;52(3):303–6. [PMID: 30105427]
Wang JB et al. Cigarette and e-cigarette dual use and risk of cardiopulmonary symptoms in the Health eHeart Study. PLoS One. 2018 Jul 25;13(7):e0198681. [PMID: 30044773]
LOWER EXTREMITY EDEMA
ESSENTIAL INQUIRIES

 History of venous thromboembolism.
History of venous thromboembolism.
 Symmetry of swelling.
Symmetry of swelling.
 Pain.
Pain.
 Change with dependence.
Change with dependence.
 Skin findings: hyperpigmentation, stasis dermatitis, lipodermatosclerosis, atrophie blanche, ulceration.
Skin findings: hyperpigmentation, stasis dermatitis, lipodermatosclerosis, atrophie blanche, ulceration.
 General Considerations
General Considerations
Acute and chronic lower extremity edema present important diagnostic and treatment challenges. Lower extremities can swell in response to increased venous or lymphatic pressures, decreased intravascular oncotic pressure, increased capillary leak, and local injury or infection. Chronic venous insufficiency is by far the most common cause, affecting up to 2% of the population, and the incidence of venous insufficiency has not changed over the past 25 years. Venous insufficiency is a common complication of DVT; however, only a small number of patients with chronic venous insufficiency report a history of this disorder. Venous ulceration commonly affects patients with chronic venous insufficiency, and its management is labor-intensive and expensive. Normal lower extremity venous pressure (in the erect position: 80 mm Hg in deep veins, 20–30 mm Hg in superficial veins) and cephalad venous blood flow require competent bicuspid venous valves, effective muscle contractions, normal ankle range of motion, and normal respirations. When one or more of these components fail, venous hypertension may result. Chronic exposure to elevated venous pressure by the postcapillary venules in the legs leads to leakage of fibrinogen and growth factors into the interstitial space, leukocyte aggregation and activation, and obliteration of the cutaneous lymphatic network.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
1. Unilateral lower extremity edema—Among common causes of unilateral lower extremity swelling, DVT is the most life-threatening. Clues suggesting DVT include a history of cancer, recent limb immobilization, or confinement to bed for at least 3 days following major surgery within the past month (Table 2–4). Adults with varicose veins have a significantly increased risk of DVT. Lower extremity swelling and inflammation in a limb recently affected by DVT could represent anticoagulation failure and thrombus recurrence but more often are caused by postphlebitic syndrome with valvular incompetence. A search for alternative explanations is equally important in excluding DVT. Other causes of a painful, swollen calf include cellulitis, musculoskeletal disorders (Baker cyst rupture [“pseudothrombophlebitis”]), gastrocnemius tear or rupture, calf strain or trauma, and left common iliac vein compression (May-Thurner syndrome), as well as other sites of nonthrombotic venous outflow obstruction, such as the inguinal ligament, iliac bifurcation, and popliteal fossa. Swelling of the ankle can be a manifestation of Charcot neuropathic osteoarthropathy.
Table 2–4. Risk stratification of adults referred for ultrasound to rule out DVT.

2. Bilateral lower extremity edema—Bilateral involvement and significant improvement upon awakening favor systemic causes (eg, venous insufficiency) and can be presenting symptoms of volume overload (HF, cirrhosis, kidney disease [eg, nephrotic syndrome]). The sensation of “heavy legs” is the most frequent symptom of chronic venous insufficiency, followed by itching. Chronic exposure to elevated venous pressure accounts for the brawny, fibrotic skin changes observed in patients with chronic venous insufficiency as well as the predisposition toward skin ulceration, particularly in the medial malleolar area. Pain, particularly if severe, is uncommon in uncomplicated venous insufficiency.
Lower extremity swelling is a familiar complication of therapy with calcium channel blockers (particularly felodipine and amlodipine), pioglitazone, gabapentin, and minoxidil. Prolonged airline flights (longer than 10 hours) are associated with edema even in the absence of DVT. Lymphedema and lipedema are other causes of bilateral lower extremity edema.
B. Physical Examination
Physical examination should include assessment of the heart, lungs, and abdomen for evidence of pulmonary hypertension (primary or secondary to chronic lung disease), HF, or cirrhosis. Some patients with cirrhosis have pulmonary hypertension without lung disease. There is a spectrum of skin findings related to chronic venous insufficiency that depends on the severity and chronicity of the disease, ranging from hyperpigmentation and stasis dermatitis to abnormalities highly specific for chronic venous insufficiency: lipodermatosclerosis (thick, brawny skin; in advanced cases, the lower leg resembles an inverted champagne bottle) and atrophie blanche (small depigmented macules within areas of heavy pigmentation). The size of both calves should be measured 10 cm below the tibial tuberosity and pitting and tenderness elicited. Leg edema may also be measured by ultrasonography with a gel pad if physical examination is equivocal. Swelling of the entire leg or of one leg 3 cm more than the other suggests deep venous obstruction. The left calf is normally slightly larger than the right as a result of the left common iliac vein coursing under the aorta.
An ulcer located over the medial malleolus is a hallmark of chronic venous insufficiency but can be due to other causes. Shallow, large, modestly painful ulcers are characteristic of venous insufficiency, whereas small, deep, and more painful ulcers are more apt to be due to arterial insufficiency, vasculitis, or infection (including cutaneous diphtheria). Diabetic vascular ulcers, however, may be painless. When an ulcer is on the foot or above the mid-calf, causes other than venous insufficiency should be considered.
The physical examination is usually inadequate to distinguish lymphedema from venous insufficiency. Sensitivity and specificity of clinical signs in predicting lymphoscintigraphy-confirmed lymphedema were 17% and 88%, respectively. Only the Kaposi-Stemmer sign (the inability to pinch or pick up a fold of skin at the base of the second toe because of its thickness) was a significant predictor of lymphedema (odds ratio, 7.9; P = 0.02).
C. Diagnostic Studies
Patients without an obvious cause of acute lower extremity swelling (eg, calf strain) should have an ultrasound performed, since DVT is difficult to exclude on clinical grounds. A prediction rule allows a clinician to exclude a lower extremity DVT in patients without an ultrasound if the patient has low pretest probability for DVT and a negative sensitive D-dimer test (the “Wells prediction rule”). The diagnostic study of choice to detect chronic venous insufficiency due venous incompetence is duplex ultrasonography. Assessment of the ankle-brachial pressure index (ABPI) is important in the management of chronic venous insufficiency, since peripheral arterial disease may be exacerbated by compression therapy. This can be performed at the same time as ultrasound. Caution is required in interpreting the results of ABPI in older patients and diabetics due to the decreased compressibility of their arteries. A urine dipstick test that is strongly positive for protein can suggest nephrotic syndrome, and a serum creatinine can help estimate kidney function. Lymphoscintigraphy can be used to confirm a clinical suspicion of lymphedema. Ambulatory sensors for measuring circumference of lower limbs to assist management of chronic venous insufficiency and lymphedema are being developed.
 Treatment
Treatment
Treatment of lower extremity edema should be guided by the underlying cause. See relevant chapters for treatment of edema in patients with HF (Chapter 10), nephrosis (Chapter 22), cirrhosis (Chapter 16), and lymphedema and venous stasis ulcers (Chapter 12). Edema resulting from calcium channel blocker therapy responds to concomitant therapy with ACE inhibitors or angiotensin receptor blockers.
In patients with chronic venous insufficiency without a comorbid volume overload state (eg, HF), it is best to avoid diuretic therapy. These patients have relatively decreased intravascular volume, and administration of diuretics may first enhance sodium retention through increased secretion of renin and angiotensin and then result in acute kidney injury and oliguria. Instead, the most effective treatment involves (1) leg elevation, above the level of the heart, for 30 minutes three to four times daily, and during sleep; (2) compression therapy; and (3) ambulatory exercise to increase venous return through calf muscle contractions. There is no evidence for benefit or harm of valvuloplasty in the treatment of patients with deep venous insufficiency secondary to primary valvular incompetence.
A wide variety of stockings and devices are effective in decreasing swelling and preventing ulcer formation. They should be put on with awakening, before hydrostatic forces result in edema. To control simple edema, 20–30 mm Hg compression is usually sufficient, whereas 30–40 mm Hg compression is usually required to control moderate to severe edema associated with ulcer formation. To maintain improvement, consider switching from an elastic stocking to one made of inelastic grosgrain material. Patients with decreased ABPI should be managed in concert with a vascular surgeon. Compression stockings (12–18 mm Hg at the ankle) are effective in preventing edema and asymptomatic thrombosis associated with long airline flights in low- to medium-risk persons. Support stockings are recommended for pregnant women during air travel. For lymphedema, bandaging systems applied twice weekly can be effective. Short-term manual lymphatic drainage treatment may improve chronic venous insufficiency severity, symptoms, and quality of life. For patients with reduced mobility and leg edema, intermittent pneumatic compression treatment can reduce edema and improve ankle range of motion.
Liposuction, suction-assisted lipectomy, and subcutaneous drainage may have treatment benefit if conservative measures fail in treatment of lymphedema.
 When to Refer
When to Refer
• Refer patients with chronic lower extremity ulcerations requiring specialist wound care.
• Refer patients with nephrotic syndrome to a nephrologist.
• Refer patients with coexisting severe arterial insufficiency (claudication) that would complicate treatment with compression stockings to a vascular surgeon.
 When to Admit
When to Admit
• Pending definitive diagnosis in patients at high risk for DVT despite normal lower extremity ultrasound.
• Severe, acute swelling raising concern for an impending compartment syndrome.
• Severe edema that impairs ability to ambulate or perform activities of daily living.
Bonkemeyer Millan S et al. Venous ulcers: diagnosis and treatment. Am Fam Physician. 2019 Sep 1;100(5):298–305. [PMID: 31478635]
Chang SL et al. Association of varicose veins with incident venous thromboembolism and peripheral artery disease. JAMA. 2018 Feb 27;319(8):807–17. [PMID: 29486040]
Garcia R et al. Duplex ultrasound for the diagnosis of acute and chronic venous diseases. Surg Clin North Am. 2018 Apr;98(2):201–18. [PMID: 29502767]
Jayaraj A et al. The diagnostic unreliability of classic physical signs of lymphedema. J Vasc Surg Venous Lymphat Disord. 2019 Nov;7(6):890–7. [PMID: 31281100]
Raffetto JD. Pathophysiology of chronic venous disease and venous ulcers. Surg Clin North Am. 2018 Apr;98(2):337–47. [PMID: 29502775]
FEVER & HYPERTHERMIA
ESSENTIAL INQUIRIES

 Age; injection substance use.
Age; injection substance use.
 Localizing symptoms; weight loss; joint pain.
Localizing symptoms; weight loss; joint pain.
 Immunosuppression or neutropenia; history of cancer.
Immunosuppression or neutropenia; history of cancer.
 Medications.
Medications.
 Travel.
Travel.
 General Considerations
General Considerations
The average normal oral body temperature taken in mid-morning is 36.7°C (range 36–37.4°C). This range includes a mean and 2 standard deviations, thus encompassing 95% of a normal population (normal diurnal temperature variation is 0.5–1°C). The normal rectal or vaginal temperature is 0.5°C higher than the oral temperature, and the axillary temperature is 0.5°C lower. Interestingly, in a pooled meta-analysis comparing peripheral with central body temperature measurement, peripheral thermometers (tympanic membrane, temporal artery, axillary, oral) showed low sensitivity but high specificity. This suggests that a normal body temperature based on a peripheral measurement does not always exclude the presence of a fever. Thus, to exclude a fever, a rectal temperature is more reliable than an oral temperature (particularly in patients who breathe through their mouth or are tachypneic or who are in an intensive care unit setting where a rectal temperature probe can be placed to detect fever). Wearable digital thermometers may detect early mild increased temperature in patients with low white blood cell counts.
Fever is a regulated rise to a new “set point” of body temperature in the hypothalamus induced by pyrogenic cytokines. These cytokines include interleukin-1 (IL-1), tumor necrosis factor (TNF), interferon-gamma, and interleukin-6 (IL-6). The elevation in temperature results from either increased heat production (eg, shivering) or decreased heat loss (eg, peripheral vasoconstriction). Body temperature in cytokine-induced fever seldom exceeds 41.1°C unless there is structural damage to hypothalamic regulatory centers.
 Clinical Findings
Clinical Findings
A. Fever
Fever as a symptom provides important information about the presence of illness—particularly infections—and about changes in the clinical status of the patient. Fever may be more predictive of bacteremia in elderly patients. The fever pattern, however, is of marginal value for most specific diagnoses except for the relapsing fever of malaria, borreliosis, and occasional cases of lymphoma, especially Hodgkin disease. Furthermore, the degree of temperature elevation does not necessarily correspond to the severity of the illness. Contrary to common perceptions, a Swedish study found that increased body temperature in the emergency department was strongly associated with lower mortality and shorter hospital stays in patients with severe sepsis or septic shock subsequently admitted to the intensive care unit even after adjustment for quality of care measures. Fever, with rash and eosinophilia, define the drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome.
In general, the febrile response tends to be greater in children than in adults. In older persons, neonates, and persons receiving certain medications (eg, nonsteroidal anti-inflammatory drugs [NSAIDs], corticosteroids), a normal temperature or even hypothermia may be observed. Markedly elevated body temperature may result in profound metabolic disturbances. High temperature during the first trimester of pregnancy may cause birth defects, such as anencephaly. Fever increases insulin requirements and alters the metabolism and disposition of drugs used for the treatment of the diverse diseases associated with fever.
The source of fever varies by population and setting. In a study involving patients who underwent shoulder arthroplasty, fever was documented in 92 patients. Among these 92 patients, an infectious cause was found in only 6 patients. In the neurointensive care unit, fever can occur directly from brain injury (called “central fever”). One model predicted “central fever” with 90% probability if a patient met all of the following criteria: (1) less than 72 hours of neurologic intensive care unit admission; (2) presence of subarachnoid hemorrhage, intraventricular hemorrhage, or brain tumor; (3) absence of infiltrate on chest radiograph; and (4) negative cultures.
Fever may also be more common in patients with other forms of trauma. In a study enrolling 268 patients, including patients with multiple injuries (n = 59), isolated head injuries (n = 97), isolated body injuries (n = 100), and minor trauma (n = 12), the incidence of fever was similar in all groups irrespective of injury (11–24%). In all groups, there was a significant association between the presence of early fever and death in the hospital (6–18% versus 0–3%), as well as longer median intensive care unit stays (3–7 days versus 2–3 days).
Among pregnant women, the prevalence of intrapartum fever of 38°C or greater in pregnancies of 36 weeks’ gestation or more is 6.8% (or 1 in 15 women in labor). And the neonatal sepsis rate among affected mothers is 0.24% (or less than 1 in 400 babies). This finding calls into question the need for universal laboratory work, cultures, and antibiotic treatment pending culture results for this newborn population.
There is increasing evidence that postoperative atelectasis does not cause fever. However, febrile nonhemolytic transfusion reaction is common, occurring in about 1% of transfusion episodes, and is mediated by proinflammatory cytokines elaborated by donor leukocytes during storage.
B. Hyperthermia
Hyperthermia—not mediated by cytokines—occurs when body metabolic heat production (as in thyroid storm) or environmental heat load exceeds normal heat loss capacity or when there is impaired heat loss; heat stroke is an example. Body temperature may rise to levels (more than 41.1°C) capable of producing irreversible protein denaturation and resultant brain damage; no diurnal variation is observed.
Malignant catatonia is a disorder consisting of catatonic symptoms, hyperthermia, autonomic instability, and altered mental status.
Neuroleptic malignant syndrome, a variant of malignant catatonia, is a rare and potentially lethal idiosyncratic reaction to neuroleptic medications, particularly haloperidol and fluphenazine; however, it has also been reported with the atypical neuroleptics (such as olanzapine or risperidone) (see Chapter 25). Serotonin syndrome resembles neuroleptic malignant syndrome but occurs within hours of ingestion of agents that increase levels of serotonin in the central nervous system, including serotonin reuptake inhibitors, monoamine oxidase inhibitors, tricyclic antidepressants, meperidine, dextromethorphan, bromocriptine, tramadol, lithium, and psychostimulants (such as cocaine, methamphetamine, and MDMA) (see Chapter 38). Clonus and hyperreflexia are more common in serotonin syndrome, whereas “lead pipe” rigidity is more common in neuroleptic malignant syndrome. Neuroleptic malignant and serotonin syndromes share common clinical and pathophysiologic features with malignant hyperthermia of anesthesia (see Chapter 38).
C. Fever of Undetermined Origin
See Fever of Unknown Origin, Chapter 30.
 Treatment
Treatment
Most fever is well tolerated. When the temperature is less than 40°C, symptomatic treatment only is required. A temperature greater than 41°C is likely to be hyperthermia rather than cytokine mediated, and emergent management is indicated. (See Heat Stroke, Chapter 37.) The treatment of fever with antipyretics does not appear to affect mortality of critically ill patients or affect the number of intensive care unit–free days.
A. General Measures for Removal of Heat
Regardless of the cause of the fever, alcohol sponges, cold sponges, ice bags, ice-water enemas, and ice baths will lower body temperature (see Chapter 37). They are more useful in hyperthermia, since patients with cytokine-related fever will attempt to override these therapies.
B. Pharmacologic Treatment of Fever
1. Antipyretic drugs—Antipyretic therapy is not needed except for patients with marginal hemodynamic status. Early administration of acetaminophen to treat fever due to probable infection did not affect the number of intensive care unit–free days. Aspirin or acetaminophen, 325–650 mg every 4 hours, is effective in reducing fever. These drugs are best administered around the clock, rather than as needed, since “as needed” dosing results in periodic chills and sweats due to fluctuations in temperature caused by varying levels of drug.
2. Antimicrobial therapy—Antibacterial and antifungal prophylactic regimens are recommended only for patients expected to have less than 100 neutrophils/mcL for more than 7 days, unless other factors increase risks for complications or mortality. In most febrile patients, empiric antibiotic therapy should be deferred pending further evaluation. However, empiric antibiotic therapy is sometimes warranted. Prompt broad-spectrum antimicrobials are indicated for febrile patients who are clinically unstable, even before infection can be documented. These include patients with hemodynamic instability, those with severe neutropenia (neutrophils less than 500/mcL), others who are asplenic (surgically or secondary to sickle cell disease) or immunosuppressed (including individuals taking systemic corticosteroids, azathioprine, cyclosporine, or other immunosuppressive medications) (Tables 30–4 and 30–5), and those who are HIV infected (see Chapter 31).
Febrile neutropenic patients should receive initial doses of empiric antibacterial therapy within an hour of triage and should either be monitored for at least 4 hours to determine suitability for outpatient management or be admitted to the hospital (see Infections in the Immunocompromised Patient, Chapter 30). Inpatient treatment is standard to manage febrile neutropenic episodes, although carefully selected patients may be managed as outpatients after systematic assessment beginning with a validated risk index (eg, Multinational Association for Supportive Care in Cancer [MASCC] score or Talcott rules). In the MASCC index calculation, low-risk factors include the following: age under 60 years (2 points), burden of illness (5 points for no or mild symptoms and 3 points for moderate symptoms), outpatient status (3 points), solid tumor or hematologic malignancy with no previous fungal infection (4 points), no COPD (4 points), no dehydration requiring parenteral fluids (3 points), and systolic blood pressure greater than 90 mm Hg (5 points). Patients with MASCC scores 21 or higher or in Talcott group 4 (presentation as an outpatient without significant comorbidity or uncontrolled cancer), and without other risk factors, can be managed safely as outpatients.
The carefully selected outpatients determined to be at low risk by MASCC score (particularly in combination with a normal serum C-reactive protein level) or by Talcott rules can be managed with an oral fluoroquinolone plus amoxicillin/clavulanate (or clindamycin, if penicillin allergic), unless fluoroquinolone prophylaxis was used before fever developed. For treatment of fever during neutropenia following chemotherapy, outpatient parenteral antimicrobial therapy can be provided effectively and safely in low-risk patients with a single agent such as cefepime, piperacillin/tazobactam, imipenem, meropenem, or doripenem. High-risk patients should be referred for inpatient management with combination parenteral antimicrobial therapy based on specific risk factors such as pneumonia-causing pathogens or central line–associated bloodstream infections (see Infections in the Immunocompromised Patient and Table 30–5 in Chapter 30, and see Infections in Chapter 39).
If a fungal infection is suspected in patients with prolonged fever and neutropenia, fluconazole is an equally effective but less toxic alternative to amphotericin B.
C. Treatment of Hyperthermia
Discontinuation of the offending agent is mandatory. Treatment of neuroleptic malignant syndrome includes dantrolene in combination with bromocriptine or levodopa (see Chapter 25). Treatment of serotonin syndrome includes administration of a central serotonin receptor antagonist—cyproheptadine or chlorpromazine—alone or in combination with a benzodiazepine (see Chapter 38). In patients for whom it is difficult to distinguish which syndrome is present, treatment with a benzodiazepine may be the safest therapeutic option.
 When to Admit
When to Admit
• Presence of additional vital sign abnormalities or evidence of end-organ dysfunction in clinical cases when early sepsis is suspected.
• For measures to control a temperature higher than 41°C or when fever is associated with seizure or other mental status changes.
• Heat stroke (see Chapter 37).
• Malignant catatonia; neuroleptic malignant syndrome; serotonin syndrome; malignant hyperthermia of anesthesia.
Copeland-Halperin LR et al. Clinical predictors of positive postoperative blood cultures. Ann Surg. 2018 Feb;267(2):297–302. [PMID: 27893534]
Hinson HE et al. Early fever after trauma: does it matter? J Trauma Acute Care Surg. 2018 Jan;84(1):19–24. [PMID: 28640776]
INVOLUNTARY WEIGHT LOSS
ESSENTIAL INQUIRIES

 Age; caloric intake; secondary confirmation (eg, changes in clothing size).
Age; caloric intake; secondary confirmation (eg, changes in clothing size).
 Fever; change in bowel habits.
Fever; change in bowel habits.
 Substance abuse.
Substance abuse.
 Age-appropriate cancer screening history.
Age-appropriate cancer screening history.
 General Considerations
General Considerations
Body weight is determined by a person’s caloric intake, absorptive capacity, metabolic rate, and energy losses. Body weight normally peaks by the fifth or sixth decade and then gradually declines at a rate of 1–2 kg per decade. In NHANES II, a national survey of community-dwelling elders (aged 50–80 years), recent involuntary weight loss (more than 5% usual body weight) was reported by 7% of respondents, and this was associated with a 24% higher mortality. In contrast, one study found that a body mass index of 33 or less is not associated with an increased mortality in adults aged 65 years or older. In postmenopausal women, unintentional weight loss was associated with increased rates of hip and vertebral fractures.
 Etiology
Etiology
Involuntary weight loss is regarded as clinically significant when it exceeds 5% or more of usual body weight over a 6- to 12-month period. It often indicates serious physical or psychological illness. Physical causes are usually evident during the initial evaluation. The most common causes are cancer (about 30%), gastrointestinal disorders (about 15%), and dementia or depression (about 15%). Nearly half of patients with Parkinson disease have weight loss associated with disease progression. When an adequately nourished–appearing patient complains of weight loss, inquiry should be made about exact weight changes (with approximate dates) and about changes in clothing size. Family members can provide confirmation of weight loss, as can old documents such as driver’s licenses. A mild, gradual weight loss occurs in some older individuals because of decreased energy requirements. However, rapid involuntary weight loss is predictive of morbidity and mortality. In addition to various disease states, causes in older individuals include loss of teeth and consequent difficulty with chewing, medications interfering with taste or causing nausea, alcoholism, and social isolation.
 Clinical Findings
Clinical Findings
Once the weight loss is established, the history, medication profile, physical examination, and conventional laboratory and radiologic investigations (eg, complete blood count, liver biochemical tests, kidney panel, serologic tests including HIV, thyroid-stimulating hormone [TSH] level, urinalysis, fecal occult blood test, chest radiography, and upper gastrointestinal series) usually reveal the cause. Whole-body CT imaging is increasingly used for diagnosis; one study found its diagnostic yield to be 33.5%. When these tests are normal, the second phase of evaluation should focus on more definitive gastrointestinal investigation (eg, tests for malabsorption, endoscopy) and cancer screening (eg, Papanicolaou smear, mammography, prostate-specific antigen [PSA]). However, one prospective case study in patients with unintentional weight loss showed that colonoscopy did not find colorectal cancer if weight loss was the sole indication for the test.
If the initial evaluation is unrevealing, follow-up is preferable to further diagnostic testing. Death at 2-year follow-up was not nearly as common in patients with unexplained involuntary weight loss (8%) as in those with weight loss due to malignant (79%) and established nonmalignant diseases (19%). Psychiatric consultation should be considered when there is evidence of depression, dementia, anorexia nervosa, or other emotional problems. Ultimately, in approximately 15–25% of cases, no cause for the weight loss can be found.
 Differential Diagnosis
Differential Diagnosis
Malignancy, gastrointestinal disorders (poorly fitting dentures, cavities, swallowing or malabsorption disorders, pancreatic insufficiency), HF, psychological problems (dementia, depression, paranoia), endocrine disorders (hyperthyroidism, hypothyroidism, hyperparathyroidism, hypoadrenalism), eating problems (dietary restrictions, lack of money for food), social problems (alcohol use disorder, social isolation), and medication side effects are all established causes.
 Treatment
Treatment
Weight stabilization occurs in most surviving patients with both established and unknown causes of weight loss through treatment of the underlying disorder and caloric supplementation. Nutrient intake goals are established in relation to the severity of weight loss, in general ranging from 30 to 40 kcal/kg/day. In order of preference, route of administration options include oral, temporary nasojejunal tube, or percutaneous gastric or jejunal tube. Parenteral nutrition is reserved for patients with serious associated problems. A variety of pharmacologic agents have been proposed for the treatment of weight loss. These can be categorized into appetite stimulants (corticosteroids, progestational agents, dronabinol, and serotonin antagonists); anabolic agents (growth hormone and testosterone derivatives); and anticatabolic agents (omega-3 fatty acids, pentoxifylline, hydrazine sulfate, and thalidomide). There is no evidence that appetite stimulants decrease mortality, and they may have severe adverse side effects. Exercise training may prevent or even reverse the process of muscle wasting in HF (“cardiac cachexia”). Protein supplementation combined with resistance exercise training and aerobic activity may prevent aging-related muscle mass attenuation and functional performance. Some patients with cancer-associated weight loss may benefit from nutritional assessment and intervention as decreased food intake may be playing a role.
 When to Refer
When to Refer
• Weight loss caused by malabsorption.
• Persistent nutritional deficiencies despite adequate supplementation.
• Weight loss as a result of anorexia or bulimia.
 When to Admit
When to Admit
• Severe protein-energy malnutrition, including the syndromes of kwashiorkor and marasmus.
• Vitamin deficiency syndromes.
• Cachexia with anticipated progressive weight loss secondary to unmanageable psychiatric disease.
• Careful electrolyte and fluid replacement in protein-energy malnutrition and avoidance of “re-feeding syndrome.”
Goh Y et al. Diagnostic utility of whole body CT scanning in patients with unexplained weight loss. PLoS One. 2018 Jul 27;13(7):e0200686. [PMID: 30052642]
Martin L et al. How much does reduced food intake contribute to cancer-associated weight loss? Curr Opin Support Palliat Care. 2018 Dec;12(4):410–9. [PMID: 30124527]
Molfino A et al. Nutrition support for treating cancer-associated weight loss: an update. Curr Opin Support Palliat Care. 2018 Dec;12(4):434–8. [PMID: 30382948]
FATIGUE & CHRONIC FATIGUE SYNDROME
ESSENTIAL INQUIRIES

 Weight loss; fever.
Weight loss; fever.
 Sleep-disordered breathing.
Sleep-disordered breathing.
 Medications; substance use.
Medications; substance use.
 General Considerations
General Considerations
Fatigue, as an isolated symptom, accounts for 1–3% of visits to generalists. The symptom of fatigue is often poorly described and less well defined by patients than symptoms associated with specific dysfunction of organ systems. Fatigue or lassitude and the closely related complaints of weakness, tiredness, and lethargy are often attributed to overexertion, poor physical conditioning, sleep disturbance, obesity, undernutrition, and emotional problems. A history of the patient’s daily living and working habits may obviate the need for extensive and unproductive diagnostic studies.
The diagnosis of chronic fatigue syndrome remains hotly debated because of the lack of a gold standard. Persons with chronic fatigue syndrome meeting specific criteria (such as those from the Centers for Disease Control and Prevention) report a greater frequency of childhood trauma and psychopathology and demonstrate higher levels of emotional instability and self-reported stress than persons who do not have chronic fatigue. Neuropsychological and neuroendocrine studies reveal abnormalities in most patients but no consistent pattern. Sleep disorders have been reported in 40–80% of patients with chronic fatigue syndrome, but polysomnographic studies have not shown a greater incidence of primary sleep disorders in those with chronic fatigue syndrome than in controls, suggesting that the sleep disorders are comorbid rather than causative. Older patients with chronic fatigue syndrome demonstrate a greater disease impact than younger patients. A retrospective cohort study in Germany found an increased risk of chronic fatigue syndrome after a first-time diagnosis of gastrointestinal infection (hazard ratio, 1.35–1.82). The phenomenon of central sensitization is a potential cause.
 Clinical Findings
Clinical Findings
A. Fatigue
Clinically relevant fatigue is composed of three major components: generalized weakness (difficulty in initiating activities); easy fatigability (difficulty in completing activities); and mental fatigue (difficulty with concentration and memory). Important diseases that can cause fatigue include hyperthyroidism and hypothyroidism, HF, infections (endocarditis, hepatitis), COPD, sleep apnea, anemia, autoimmune disorders, multiple sclerosis, irritable bowel syndrome, Parkinson disease, cerebral vascular accident, and cancer. Solution-focused therapy has a significant initial beneficial effect on the severity of fatigue and quality of life in patients with quiescent inflammatory bowel disease.
Alcohol use disorder, vitamin C deficiency (scurvy), side effects from medications (eg, sedatives and beta-blockers), and psychological conditions (eg, insomnia; depression; anxiety; panic attacks; dysthmia; and somatic symptom disorder, formerly called somatization disorder) may be the cause. Common outpatient infectious causes include mononucleosis and sinusitis. These conditions are usually associated with other characteristic signs, but patients may emphasize fatigue and not reveal their other symptoms unless directly asked. The lifetime prevalence of significant fatigue (present for at least 2 weeks) is about 25%. Fatigue of unknown cause or related to psychiatric illness exceeds that due to physical illness, injury, alcohol, or medications.
Although frequently associated with Lyme disease, severe fatigue as a long-term sequela is rare.
B. Chronic Fatigue Syndrome/Systemic Exertion Intolerance Disease
A working case definition of chronic fatigue syndrome indicates that it is not a homogeneous abnormality, there is no single pathogenic mechanism (Figure 2–1), and no physical finding or laboratory test can be used to confirm the diagnosis. Other conditions identified as causing chronic fatigue include myalgic encephalitis and neurasthenia, each with specific diagnostic criteria creating inconsistent diagnoses and treatment plans. In 2015, the Institute of Medicine (now called the National Academy of Medicine) recommended using the term systemic exertion intolerance disease (SEID). Diagnosis of SEID requires the presence of all of the following three symptoms:
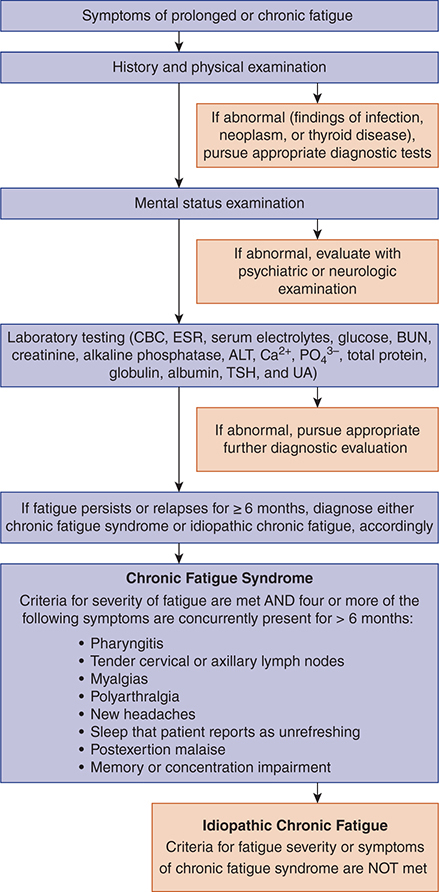
Figure 2–1. Classification of chronic fatigue patients. ALT, alanine aminotransferase; BUN, blood urea nitrogen; Ca2+, calcium; CBC, complete blood count; ESR, erythrocyte sedimentation rate; PO43–, phosphate; TSH, thyroid-stimulating hormone; UA, urinalysis.
1. Substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities that persists for more than 6 months and is accompanied by fatigue, which is often profound, is of new or definite onset (not lifelong), is not the result of ongoing excessive exertion, and is not substantially alleviated by rest.
2. Postexertional malaise.
3. Unrefreshing sleep.
In addition, the patient must have at least one of the following two manifestations: (1) cognitive impairment or (2) orthostatic intolerance (lightheadedness, dizziness, and headache that worsen with upright posture and improve with recumbency).
The evaluation of chronic fatigue syndrome or SEID includes a history and physical examination as well as complete blood count, erythrocyte sedimentation rate, chemistries (blood urea nitrogen [BUN], serum electrolytes, glucose, creatinine, calcium, liver biochemical tests, and thyroid function tests), urinalysis, tuberculin skin test, and screening questionnaires for psychiatric disorders. Other tests to be performed as clinically indicated are serum cortisol, antinuclear antibody, rheumatoid factor, immunoglobulin levels, Lyme serology in endemic areas (although rarely a long-term complication of this infection), and HIV antibody. More extensive testing is usually unhelpful, including antibody to Epstein-Barr virus. There may be an abnormally high rate of postural hypotension. Brain MRI is not routinely recommended.
 Treatment
Treatment
A. Fatigue
Management of fatigue involves identification and treatment of conditions that contribute to fatigue, such as cancer, pain, depression, disordered sleep, weight loss, and anemia. Resistance training and aerobic exercise lessens fatigue and improves performance for a number of chronic conditions associated with a high prevalence of fatigue, including HF, COPD, arthritis, and cancer. Continuous positive airway pressure is an effective treatment for obstructive sleep apnea. Psychostimulants such as methylphenidate have shown inconsistent results in randomized trials of treatment of cancer-related fatigue. Modafinil and armodafinil appear to be effective, well-tolerated agents in HIV-positive patients with fatigue and as adjunctive agents in patients with depression or bipolar disorder with fatigue. Testosterone replacement in hypoandrogenic men over age 65 had no significant benefit with respect to walking distance or vitality, as assessed by the Functional Assessment of Chronic Illness Therapy-Fatigue scale, but men who received the testosterone reported slightly better mood and lower severity of depressive symptoms than those who received placebo.
Therapeutic Care (a complementary medicine modality that uses acupressure) reduces fatigue in some patients with breast cancer receiving chemotherapy, and Internet-based cognitive-behavioral therapy is effective in reducing severe fatigue in breast cancer survivors. Six weeks of Swedish massage therapy reduced fatigue in female breast cancer survivors who had surgery plus radiation and/or chemotherapy/chemoprevention.
Methylphenidate, as well as cognitive-behavioral therapy, may improve mental fatigue and cognitive functions in patients with traumatic brain injury. The TRUST study found that treatment of subclinical hypothyroidism with levothyroxine did not improve symptoms of fatigue as measured by the Tiredness score (3.2±17.7 in placebo group and 3.8 in levothyroxine group ±18.4, respectively; between-group difference, 0.4; 95% CI, –2.1 to +2.9). Vitamin D treatment significantly improved fatigue in kidney transplantation patients as well as in otherwise healthy persons with vitamin D deficiency.
B. Chronic Fatigue Syndrome
A variety of agents and modalities have been tried for the treatment of chronic fatigue syndrome. Acyclovir, intravenous immunoglobulin, nystatin, clonidine (in adolescent chronic fatigue syndrome), peripheral IL-1 inhibition with anakinra, and low-dose hydrocortisone do not improve symptoms. Inhibition of cytokine IL-1 with anakinra for 4 weeks does not result in a clinically significant reduction in fatigue severity in women with chronic fatigue syndrome. Some patients with postural hypotension report response to increases in dietary sodium as well as fludrocortisone, 0.1 mg orally daily. The immune modulator rintatolimod improved some measures of exercise performance compared with placebo in two trials (low strength of evidence). There is very limited evidence that dietary modification is beneficial.
There is a greater prevalence of past and current psychiatric diagnoses in patients with this syndrome. Affective disorders are especially common. Patients with chronic fatigue syndrome have benefited from a comprehensive multidisciplinary intervention, including optimal medical management, treating any ongoing affective or anxiety disorder pharmacologically, and implementing a comprehensive cognitive-behavioral treatment program. At present, cognitive-behavioral therapy and graded exercise are the treatments of choice for patients with chronic fatigue syndrome. Cognitive-behavioral therapy, a form of nonpharmacologic treatment emphasizing self-help and aiming to change perceptions and behaviors that may perpetuate symptoms and disability, may be helpful in some patients. Response to cognitive-behavioral therapy is not predictable on the basis of severity or duration of chronic fatigue syndrome. Patients with high neuroticism or low acceptance show more improvement in mental quality of life with cognitive-behavioral therapy.
Graded exercise may result in mild-to-moderate improvements in functional work capacity and physical function in some patients but may prove risky in others. A 2011 randomized trial (PACE trial) confirmed the independent benefits of cognitive-behavioral therapy and graded exercise, but recent meta-analyses and re-analysis of PACE are calling into question the magnitude of the benefit and safety of graded exercise. Physiologic studies find an altered immune response to exercise in patients with chronic fatigue syndrome. A self-help booklet describing a six-step graded exercise program over 12 weeks and up to four guidance sessions with a physiotherapist over 8 weeks may be as helpful as specialist medical care alone.
A critical appraisal of the Cochrane reviews addressing exercise and cognitive-behavioral therapy as treatments for chronic fatigue syndrome reports that the evidence-base is insufficient to exclude harms, and concludes that these treatments are better characterized as “adjunctive therapies.”
In addition, the clinician’s sympathetic listening and explanatory responses can help overcome the patient’s frustrations and debilitation by this still mysterious illness. All patients should be encouraged to engage in normal activities to the extent possible and should be reassured that full recovery is eventually possible in most cases. Chronic fatigue syndrome is not associated with increased all-cause mortality, but one study showed a substantially increased risk of completed suicide.
 When to Refer
When to Refer
• Infections not responsive to standard treatment.
• Difficult-to-control hyperthyroidism or hypothyroidism.
• Severe psychological illness.
• Malignancy.
 When to Admit
When to Admit
• Failure to thrive.
• Fatigue severe enough to impair activities of daily living.
Donnachie E et al. Incidence of irritable bowel syndrome and chronic fatigue following GI infection: a population-level study using routinely collected claims data. Gut. 2018 Jun;67(6):1078–86. [PMID: 28601847]
Kinkead B et al. Massage therapy decreases cancer-related fatigue: results from a randomized early phase trial. Cancer. 2018 Feb 1;124(3):546–54. [PMID: 29044466]
Komaroff AL. Advances in understanding the pathophysiology of chronic fatigue syndrome. JAMA. 2019 Aug 13;322(6):499–500. [PMID: 31276153]
Vink M et al. Cognitive behavioural therapy for myalgic encephalomyelitis/chronic fatigue syndrome is not effective. Re-analysis of a Cochrane review. Health Psychol Open. 2019 May 2;6(1):2055102919840614. [PMID: 31080632]
Wilshire CE et al. Rethinking the treatment of chronic fatigue syndrome—a reanalysis and evaluation of findings from a recent major trial of graded exercise and CBT. BMC Psychol. 2018 Mar 22;6(1):6. [PMID: 29562932]
ACUTE HEADACHE
ESSENTIAL INQUIRIES

 Age older than 40 years.
Age older than 40 years.
 Rapid onset and severe intensity (ie, “thunderclap” headache), trauma, onset during exertion.
Rapid onset and severe intensity (ie, “thunderclap” headache), trauma, onset during exertion.
 Fever, vision changes, neck stiffness.
Fever, vision changes, neck stiffness.
 HIV infection.
HIV infection.
 Current or past history of hypertension.
Current or past history of hypertension.
 Neurologic findings (mental status changes, motor or sensory deficits, loss of consciousness).
Neurologic findings (mental status changes, motor or sensory deficits, loss of consciousness).
 General Considerations
General Considerations
Headache is a common reason that adults seek medical care, accounting for approximately 13 million visits each year in the United States to physicians’ offices, urgent care clinics, and emergency departments. It is the fifth most common reason for emergency department visits, and second most common reason for neurologic consultation in the emergency department. A broad range of disorders can cause headache (see Chapter 24). This section deals only with acute nontraumatic headache in adults and adolescents. The challenge in the initial evaluation of acute headache is to identify which patients are presenting with an uncommon but life-threatening condition; approximately 1% of patients seeking care in emergency department settings and considerably less in office practice settings fall into this category.
Diminution of headache in response to typical migraine therapies (such as serotonin receptor antagonists or ketorolac) does not rule out critical conditions such as subarachnoid hemorrhage or meningitis as the underlying cause.
 Clinical Findings
Clinical Findings
A. Symptoms
A careful history and physical examination should aim to identify causes of acute headache that require immediate treatment. These causes can be broadly classified as imminent or completed vascular events (intracranial hemorrhage, thrombosis, cavernous sinus thrombosis, vasculitis, malignant hypertension, arterial dissection, cerebral venous thrombosis, transient ischemic attack, or aneurysm), infections (abscess, encephalitis, or meningitis), intracranial masses causing intracranial hypertension, preeclampsia, and carbon monoxide poisoning. Having the patient carefully describe the onset of headache can be helpful in diagnosing a serious cause. Report of a sudden-onset headache that reaches maximal and severe intensity within seconds or a few minutes is the classic description of a “thunderclap” headache; it should precipitate workup for subarachnoid hemorrhage, since the estimated prevalence of subarachnoid hemorrhage in patients with thunderclap headache is 43%. Thunderclap headache during the postpartum period precipitated by the Valsalva maneuver or recumbent positioning may indicate reversible cerebral vasoconstriction syndrome. Other historical features that raise the need for diagnostic testing include headache brought on by the Valsalva maneuver, cough, exertion, or sexual activity.
The medical history can also guide the need for additional workup. Under most circumstances (including a normal neurologic examination), new headache in a patient older than 50 years or with HIV infection warrants immediate neuroimaging (Table 2–5). When the patient has a history of hypertension—particularly uncontrolled hypertension—a complete search for other features of “malignant hypertension” is appropriate to determine the urgency of control of hypertension (see Chapter 11). Headache and hypertension associated with pregnancy may be due to preeclampsia. Episodic headache associated with the triad of hypertension, palpitations, and sweats is suggestive of pheochromocytoma. In the absence of thunderclap headache, advanced age, and HIV infection, a careful physical examination and detailed neurologic examination will usually determine acuity of the workup and need for further diagnostic testing. A history consistent with hypercoagulability is associated with an increased risk of cerebral venous thrombosis.
Table 2–5. Clinical features associated with acute headache that warrant urgent or emergent neuroimaging.
Prior to lumbar puncture
Abnormal neurologic examination
Abnormal mental status
Abnormal funduscopic examination (papilledema; loss of venous pulsations)
Meningeal signs
Emergent (conduct prior to leaving office or emergency department)
Abnormal neurologic examination
Abnormal mental status
“Thunderclap” headache
Urgent (scheduled prior to leaving office or emergency department)
HIV-positive patient1
Age > 50 years (normal neurologic examination)
1Use CT with or without contrast or MRI if HIV positive.
Data from American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of patients presenting to the emergency department with acute headache. Ann Emerg Med. 2002 Jan;39(1):108–22.
Symptoms can also be useful for diagnosing migraine headache in the absence of the “classic” migraine pattern of scintillating scotoma followed by unilateral headache, photophobia, and nausea and vomiting (Table 2–6). The presence of three or more of these symptoms (nausea, photophobia, phonophobia, and exacerbation by physical activity) can establish the diagnosis of migraine (in the absence of other clinical features that warrant neuroimaging studies), and the presence of only one or two symptoms (provided one is not nausea) can help rule out migraine. A systematic list called the SNNOOP10 has been developed as a screening method for secondary causes of headache (Table 2–7).
Table 2–6. Summary likelihood ratios (LRs) for individual clinical features associated with migraine diagnosis.
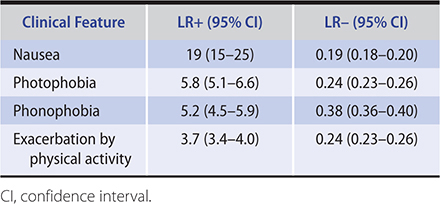
Table 2–7. SNNOOP10 list of “red” flags for secondary causes of headache.
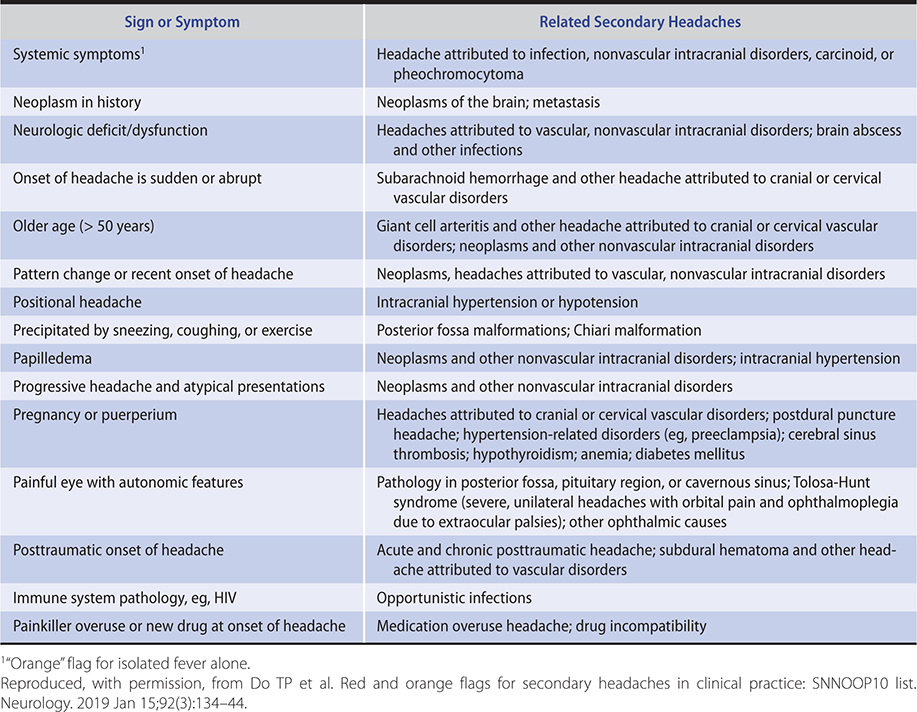
B. Physical Examination
Critical components of the physical examination of the patient with acute headache include vital signs, neurologic examination, and vision testing with funduscopic examination. The finding of fever with acute headache warrants additional maneuvers to elicit evidence of meningeal inflammation, such as Kernig and Brudzinski signs. The absence of jolt accentuation of headache cannot accurately rule out meningitis. Patients older than 60 years should be examined for scalp or temporal artery tenderness.
Careful assessment of visual acuity, ocular gaze, visual fields, pupillary defects, optic disks, and retinal vein pulsations is crucial. Diminished visual acuity is suggestive of glaucoma, temporal arteritis, or optic neuritis. Ophthalmoplegia or visual field defects may be signs of venous sinus thrombosis, tumor, or aneurysm. Afferent pupillary defects can be due to intracranial masses or optic neuritis. In the setting of headache and hypertension, retinal cotton wool spots, flame hemorrhages, and disk swelling indicate acute severe hypertensive retinopathy. Ipsilateral ptosis and miosis suggest Horner syndrome and in conjunction with acute headache may signify carotid artery dissection. Finally, papilledema or absent retinal venous pulsations are signs of elevated intracranial pressure—findings that should be followed by neuroimaging prior to performing lumbar puncture (Table 2–5). On nonmydriatic fundoscopy, up to 8.5% of patients who arrive at the emergency department complaining of headache had abnormalities; although few had other significant physical examination findings, 59% of them had abnormal neuroimaging studies.
Complete neurologic evaluations are also critical and should include assessment of mental status, motor and sensory systems, reflexes, gait, cerebellar function, and pronator drift. Any abnormality on neurologic evaluation (especially mental status) warrants emergent neuroimaging (Table 2–5).
C. Diagnostic Studies
Neuroimaging is summarized in Table 2–5. Under most circumstances, a noncontrast head CT is sufficient to exclude intracranial hypertension with impending herniation, intracranial hemorrhage, and many types of intracranial masses (notable exceptions include lymphoma and toxoplasmosis in HIV-positive patients, herpes simplex encephalitis, and brain abscess). When needed, a contrast study can be ordered to follow a normal noncontrast study. A normal neuroimaging study does not exclude subarachnoid hemorrhage and should be followed by lumbar puncture. One study supported a change of practice wherein a lumbar puncture can be withheld when a head CT scan was performed less than 6 hours after headache onset and showed no evidence of subarachnoid hemorrhage (negative predictive value 99.9% [95% CI, 99.3–100.0%]).
In patients for whom there is a high level of suspicion for subarachnoid hemorrhage or aneurysm, a normal CT and lumbar puncture should be followed by angiography within the next few days (provided the patient is medically stable). Lumbar puncture is also indicated to exclude infectious causes of acute headache, particularly in patients with fever or meningeal signs. Cerebrospinal fluid tests should routinely include Gram stain, white blood cell count with differential, red blood cell count, glucose, total protein, and bacterial culture. In appropriate patients, also consider testing cerebrospinal fluid for VDRL (syphilis), cryptococcal antigen (HIV-positive patients), acid-fast bacillus stain and culture, and complement fixation and culture for coccidioidomycosis. Storage of an extra tube with 5 mL of cerebrospinal fluid is also prudent for conducting unanticipated tests in the immediate future. Polymerase chain reaction tests for specific infectious pathogens (eg, herpes simplex 2) should also be considered in patients with evidence of central nervous system infection but no identifiable pathogen.
The Ottawa subarachnoid hemorrhage clinical decision rule had 100% sensitivity (and 13–15% specificity in different studies) in predicting subarachnoid hemorrhage. According to it, patients who seek medical attention in an emergency department complaining of an acute nontraumatic headache should be evaluated for subarachnoid hemorrhage if they have one or more of the following factors: age 40 years or older, neck pain or stiffness, witnessed loss of consciousness, onset during exertion, thunderclap headache (instantly peaking pain), or limited neck flexion on examination.
In addition to neuroimaging and lumbar puncture, additional diagnostic tests for exclusion of life-threatening causes of acute headache include erythrocyte sedimentation rate (temporal arteritis; endocarditis), urinalysis (malignant hypertension; preeclampsia), and sinus CT (bacterial sinusitis, independently or as a cause of venous sinus thrombosis).
 Treatment
Treatment
Treatment should be directed at the cause of acute headache. In patients in whom migraine or migraine-like headache has been diagnosed, early treatment with NSAIDs (oral, nasal, or intramuscular ketorolac), metoclopramide, dihydroergotamine, or triptans (oral, nasal, subcutaneous) can often abort or provide significant relief of symptoms (see Chapter 24). Intravenous prochlorperazine plus diphenhydramine was more effective for migraine pain relief than intravenous hydromorphone in the emergency department. There appears to be no benefit of adding intravenous diphenhydramine to intravenous metoclopramide. Prochlorperazine appears to be superior to ketamine for the treatment of benign headaches in the emergency department. Sumatriptan may be less effective as immediate therapy for migraine attacks with aura compared to attacks without aura. There may be a role for oral corticosteroids to prevent rebound headache after emergency department discharge. Parenteral morphine and hydromorphone are best avoided as first-line therapy.
Subanesthetic ketamine infusions may be beneficial in individuals with chronic migraine and new daily persistent headache that has not responded to other aggressive treatments. Peripheral nerve blocks may be a safe and effective way to treat headaches in older adults. Surgical decompression of peripheral cranial and spinal nerves at trigger sites have been used to treat migraine. Noninvasive vagus nerve stimulation has shown promise in the management of migraine and acute cluster headaches.
High-flow oxygen therapy may also provide effective treatment for all headache types in the emergency department setting. Peripheral nerve blocks for treatment-refractory migraine may be an effective therapeutic option in pregnancy. The oral 5-HT1F receptor agonist, lasmiditan, has been approved for the acute treatment of migraine with or without aura in adults. The CGRP monoclonal antibodies (erenumab, fremanezumab, galcanezumab) have been approved for prevention of migraine. Galcanezumab has activity against cluster headache.
Regular exercise may have a prophylactic effect on migraine frequency; however, new, intense exercise can trigger migraine.
 When to Refer
When to Refer
• Frequent migraines not responsive to standard therapy.
• Migraines with atypical features.
• Chronic daily headaches due to medication overuse.
 When to Admit
When to Admit
• Need for repeated doses of parenteral pain medication.
• To facilitate an expedited workup requiring a sequence of neuroimaging and procedures.
• To monitor for progression of symptoms and to obtain neurologic consultation when the initial emergency department workup is inconclusive.
• Pain severe enough to impair activities of daily living or impede follow-up appointments or consultations.
• Patients with subarachnoid hemorrhage, intracranial mass, or meningitis.
Burch R. Migraine and tension-type headache: diagnosis and treatment. Med Clin North Am. 2019 Mar;103(2):215–33. [PMID: 30704678]
Diamanti S et al. Leading symptoms in cerebrovascular diseases: what about headache? Neurol Sci. 2019 May;40(Suppl 1):147–52. [PMID: 30891639]
Do TP et al. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology. 2019 Jan 15;92(3):134–44. [PMID: 30587518]
Rashed A et al. Current approach to undifferentiated headache management in the emergency department. Curr Pain Headache Rep. 2019 Mar 14;23(4):26. [PMID: 30868276]
Starling AJ. Diagnosis and management of headache in older adults. Mayo Clin Proc. 2018 Feb;93(2):252–62. [PMID: 29406202]
DYSURIA
ESSENTIAL INQUIRIES

 Fever; new back or flank pain; nausea or vomiting.
Fever; new back or flank pain; nausea or vomiting.
 Vaginal discharge.
Vaginal discharge.
 Pregnancy risk.
Pregnancy risk.
 Structural abnormalities.
Structural abnormalities.
 Instrumentation of urethra or bladder.
Instrumentation of urethra or bladder.
 General Considerations
General Considerations
Dysuria (painful urination) is a common reason for adults and adolescents to seek urgent medical attention. An inflammatory process (eg, urinary tract infection [UTI], autoimmune disorder) underlies most causes of dysuria. In women, cystitis will be diagnosed in up to 50–60% of cases. Cystitis has an incidence of 0.5–0.7% per year in sexually active young women. The key objective in evaluating women with dysuria is to exclude serious upper urinary tract disease, such as acute pyelonephritis, and sexually transmitted diseases. In elderly men, dysuria may be a symptom of prostatitis. In contrast, in younger men, urethritis accounts for the vast majority of cases of dysuria. Male cyclists had no worse sexual or urinary functions than swimmers or runners, but cyclists were more prone to urethral stricture.
 Clinical Findings
Clinical Findings
A. Symptoms
Well-designed cohort studies have shown that some women can be reliably diagnosed with uncomplicated cystitis without a physical examination or urinalysis, and randomized controlled trials show that telephone management of uncomplicated cystitis is safe and effective. An increased likelihood of cystitis is present when women report multiple irritative voiding symptoms (dysuria, urgency, frequency), fever, or back pain (LRs = 1.6–2.0). A cohort study found that the symptom of dysuria most reliably predicted a culture-positive UTI. Inquiring about symptoms of vulvovaginitis is imperative. When women report dysuria and urinary frequency, and deny vaginal discharge and irritation, the LR for culture-confirmed cystitis is 24.5. In contrast, when vaginal discharge or irritation is present, as well as dysuria or urinary frequency, the LR is 0.7. Gross hematuria in women with voiding symptoms usually represents hemorrhagic cystitis but can also be a sign of bladder cancer (particularly in older patients) or upper tract disease. Failure of hematuria to resolve with antibiotic treatment should prompt further evaluation of the bladder and kidneys. Chlamydial infection should be strongly considered among women aged 25 years or younger who are sexually active and seeking medical attention for a suspected UTI for the first time or who have a new partner.
Because fever and back pain, as well as nausea and vomiting, are considered harbingers of (or clinical criteria for) acute pyelonephritis, women with these symptoms should usually be examined by a clinician prior to treatment in order to exclude coexistent urosepsis, hydronephrosis, or nephrolithiasis that would affect management decisions. Risk factors for acute pyelonephritis among women 18–49 years of age relate to sexual behaviors (frequent sexual intercourse (3 times per week or more), new sexual partner in previous year, recent spermicide use), as well as diabetes mellitus and recent UTI or incontinence. Finally, pregnancy, underlying structural factors (polycystic kidney disease, nephrolithiasis, neurogenic bladder), immunosuppression, diabetes mellitus, and a history of recent bladder or urethral instrumentation usually alter the treatment regimen (antibiotic choice or duration of treatment, or both) of cystitis. Presence of UTI during pregnancy is strongly associated with preeclampsia (particularly during the third trimester).
B. Physical Examination
Fever, tachycardia, or hypotension suggests the possibility of urosepsis and potential need for hospitalization. A focused examination in women, in uncomplicated circumstances, could be limited to ascertainment of costovertebral angle tenderness and to a lower abdominal and pelvic examination if the history suggests vulvovaginitis or cervicitis.
C. Diagnostic Studies
1. Urinalysis—Urinalysis is probably overutilized in the evaluation of dysuria. The probability of culture-confirmed UTI among women with a history and physical examination compatible with uncomplicated cystitis is about 70–90%. Urinalysis is most helpful in atypical presentations of cystitis. Dipstick detection (greater than trace) of leukocytes, nitrites, or blood supports a diagnosis of cystitis. When both leukocyte and nitrite tests are positive, the LR is 4.2, and when both are negative, the LR is 0.3. The negative predictive value of urinalysis is not sufficient to exclude culture-confirmed UTI in women with multiple and typical symptoms, and randomized trial evidence shows that antibiotic treatment is beneficial to women with typical symptoms and negative urinalysis dipstick tests. Microscopy of unspun urine may also be helpful in diagnosis and reduces unnecessary use of antibiotics. The combination of urgency, dysuria, and pyuria, assessed with the high-power objective (40 ×) for pus cells (more than 1 pus cell/7 high-power fields) had a positive predictive value of 71 and LR of 2.97.
2. Urine culture—Urine culture should be considered for all women with upper tract symptoms (prior to initiating antibiotic therapy), as well as those with dysuria and a negative urine dipstick test. In symptomatic women, a clean-catch urine culture is considered positive when 102–103 colony-forming units/mL of a uropathogenic organism is detected.
3. Renal imaging—When severe flank or back pain is present, the possibility of complicated kidney infection (perinephric abscess, nephrolithiasis) or of hydronephrosis should be considered. Renal ultrasound or CT scanning should be done to rule out abscess and hydronephrosis. To exclude nephrolithiasis, noncontrast helical CT scanning is more accurate than intravenous urography and is the diagnostic test of choice. In a meta-analysis, the positive and negative LRs of helical CT scanning for diagnosis of nephrolithiasis were 23.2 and 0.05, respectively.
 Differential Diagnosis
Differential Diagnosis
The differential diagnosis of dysuria in women includes acute cystitis, acute pyelonephritis, vaginitis (Candida, bacterial vaginosis, Trichomonas, herpes simplex), urethritis/cervicitis (Chlamydia, gonorrhea), and interstitial cystitis/painful bladder syndrome. Nucleic acid amplification tests from first-void urine or vaginal swab specimens are highly sensitive for detecting chlamydial infection. Other infectious pathogens associated with dysuria and urethritis in men include Mycoplasma genitalium and Enterobacteriaceae.
 Treatment
Treatment
Definitive treatment is directed to the underlying cause of the dysuria. An evidence-informed algorithm for managing suspected UTI in women is shown in Figure 2–2. This algorithm supports antibiotic treatment of most women with multiple and typical symptoms of UTI without performing urinalysis or urine culture. Antibiotic selection should be guided by local resistance patterns and expert-panel clinical practice guidelines; major options for uncomplicated cystitis include nitrofurantoin, cephalosporins, ciprofloxacin, fosfomycin, and trimethoprim-sulfamethoxazole. Five days of nitrofurantoin resulted in a significantly greater likelihood of clinical and microbiologic resolution than single-dose fosfomycin. According to the American Academy of Pediatrics’ Committee on Drugs, antibiotics that are usually acceptable when treating women who are breastfeeding include trimethoprim-sulfamethoxazole (unless G6PD deficiency is present), amoxicillin, nitrofurantoin, ciprofloxacin, and ofloxacin.

Figure 2–2. Proposed algorithm for evaluating women with symptoms of acute urinary tract infection (UTI). (Data from Gupta K et al; Infectious Diseases Society of America; European Society for Microbiology and Infectious Diseases. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011 Mar 1;52(5):e103–20.)
In men, prolonged treatment of UTIs (more than 7 days) out of concern for delayed clearance of infection within the prostate does not appear to reduce early or late recurrences. A 5-day course of fluoroquinolones in outpatient men with UTI is as effective as a 10-day course.
Symptomatic relief can be provided with phenazopyridine, a urinary analgesic that is available over the counter; it is used in combination with antibiotic therapy (when a UTI has been confirmed) but for no more than 2 days. Patients should be informed that phenazopyridine will cause orange/red discoloration of their urine and other body fluids (eg, some contact lens wearers have reported discoloration of their lenses). Rare cases of methemoglobinemia and hemolytic anemia have been reported, usually with overdoses or underlying kidney dysfunction. NSAIDs have also been shown to be of symptomatic benefit, but less effective than antibiotic therapy. Although some women recover from uncomplicated UTI when treated with NSAIDs alone (53% in a Norwegian study), the rate of progression to pyelonephritis was substantial. Delayed antibiotic therapy in elderly patients with UTI leads to a substantially higher rate of bloodstream infections and all-cause mortality. If a broad-spectrum antibiotic was initially prescribed empirically for UTI and urine culture results return establishing efficacy of a narrow-spectrum antibiotic, treatment should be “de-escalated” to the narrow-spectrum antimicrobial. Among premenopausal women with recurrent UTIs, increased daily water consumption decreased the mean number of cystitis episodes over a 12-month period (1.7 [95% CI, 1.5–1.8] in the increased water consumption group compared with 3.2 [95% CI, 3.0–3.4] in the control group) and reduced the number or antibiotic prescriptions received (1.9 [95% CI, 1.7–2.2] and 3.6 [95% CI, 3.3–4.0], respectively). In patients with asymptomatic renal calculi and recurrent UTIs, stone extraction eliminated infections in 50% of women.
In cases of interstitial cystitis/painful bladder syndrome (see Chapter 23), patients will often respond to a multimodal approach that may include urethral/vesicular dilation, biofeedback, cognitive-behavioral therapy, antidepressants, dietary changes, vaginal emollients, and other supportive measures. Vaginal estrogen effectively relieves urinary urgency and frequency as well as recurrent UTIs related to vulvovaginal atrophy of menopause (also known as genitourinary syndrome of menopause).
A meta-analysis found that for most people with asymptomatic bacteriuria antibiotic treatment is not beneficial and may be harmful. Antibiotic treatment benefits both pregnant women with asymptomatic bacteriuria as well as persons about to undergo urologic surgery. The USPSTF recommends screening pregnant women for asymptomatic bacteriuria by obtaining a urine culture (B recommendation). The USPSTF recommends against screening for asymptomatic bacteriuria in nonpregnant adults (D recommendation).
There were no differences in the prevalence of postoperative UTI in women who had preoperative mixed-flora urine cultures compared to no-growth preoperative urine cultures.
 When to Refer
When to Refer
• Anatomic abnormalities leading to repeated urinary infections.
• Infections associated with nephrolithiasis.
• Persistent interstitial cystitis/painful bladder syndrome.
 When to Admit
When to Admit
• Severe pain requiring parenteral medication or impairing ambulation or urination (such as severe primary herpes simplex genitalis).
• Dysuria associated with urinary retention or obstruction.
• Pyelonephritis with ureteral obstruction.
• Symptoms and signs suggesting urosepsis.
Chu CM et al. Diagnosis and treatment of urinary tract infections across age groups. Am J Obstet Gynecol. 2018 Jul;219(1):40–51. [PMID: 29305250]
Gharbi M et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all cause mortality: population-based cohort study. BMJ. 2019 Feb 27;364:l525. [PMID: 30814048]
Hooton TM et al. Effect of increased daily water intake in premenopausal women with recurrent urinary tract infections: a randomized clinical trial. JAMA Intern Med. 2018 Nov 1;178(11):1509–15. [PMID: 30285042]
Kolman KB. Cystitis and pyelonephritis: diagnosis, treatment, and prevention. Prim Care. 2019 Jun;46(2):191–202. [PMID: 31030820]
US Preventive Services Task Force; Owens DK et al. Screening for asymptomatic bacteriuria in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2019 Sep 24;322(12):1188–94. [PMID: 31550038]