Sexually Transmitted Infections
Gale R. Burstein
Age-specific rates of many sexually transmitted infections (STIs ) are highest among sexually experienced adolescents and young adults, after controlling for sexual activity. Although some STI pathogens present as STI syndromes with a specific constellation of symptoms, most are asymptomatic and only detected by a laboratory test. The approach to prevention and control of these infections lies in education, screening, and early diagnosis and treatment.
Etiology
Any adolescent who has had oral, vaginal, or anal sexual intercourse is at risk for acquiring an STI. Not all adolescents are at equal risk; physical, behavioral, and social factors contribute to the adolescent's higher risk (Table 146.1 ). Adolescents who initiate sex at a younger age, youth residing in detention facilities, youth attending sexually transmitted disease (STD) clinics, young men having sex with men, and youth who are injection drug users are at higher risk for STIs. Risky behaviors, such as sex with multiple concurrent partners or multiple sequential partners of limited duration, failure to use barrier protection consistently and correctly, and increased biologic susceptibility to infection, also contribute to risk. Although all 50 states and the District of Columbia explicitly allow minors to consent for their own sexual health services, many adolescents encounter multiple obstacles to accessing this care. Adolescents who are victims of sexual assault may not consider themselves “sexually active,” given the context of the encounter, and need reassurance, protection, and appropriate intervention when these circumstances are uncovered (see Chapter 145 ).
Epidemiology
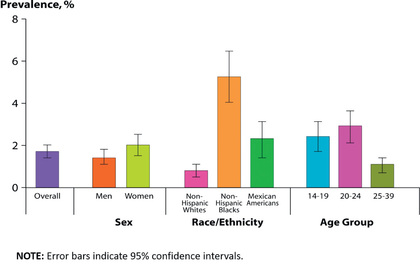
STI prevalence varies by age, gender, and race/ethnicity. In the United States, although adolescents and young adults ages 15-24 yr represent 25% of the sexually experienced population, this age-group accounts for almost 50% of all incident STIs each year. Adolescents and young adults <25 yr of age have the highest reported prevalence of gonorrhea (see Chapter 219 ) and chlamydia (see Chapter 253 ); among females and males, rates are highest in the 15-24 yr old age-groups (Fig. 146.1 ). In 2015, females age 20-24 yr had the highest reported chlamydia rate (3,730 per 100,000 population), followed by females 15-19 yr of age (2,994/100,000). The reported 2015 chlamydia rate for 15-19 yr old females was almost 4 times higher than for 15-19 yr old males. Chlamydia is common among all races and ethnic groups; Blacks, Native American/Alaska Native, and Hispanic females are disproportionately affected. In 2015, non-Hispanic black females 20-24 yr of age had the highest chlamydia rate of any group (6,783), followed by black females 15-19 yr of age (6,340). Data from the 2007–2012 National Health and Nutrition Examination Survey (NHANES) estimated the prevalence of chlamydia among the U.S. population was highest among African Americans (Fig. 146.2 ).

Reported rates of other bacterial STIs are also high among adolescents and young adults. In 2015, 20-24 yr old females had the highest (547/100,000) and 20-24 yr old males had the second highest gonorrhea rates (539/100,000) compared to any other age/sex group (see Chapter 219 ). Gonorrhea rates among 15-24 yr old males and females increased between 2014 and 2015. Syphilis rates are increasing at an alarming rate, especially among males, accounting for >90% of all primary and secondary syphilis cases. Of those male cases, men who have sex with men (MSM) account for 82% of male cases when the gender of the sex partner is known. Males age 20-24 yr have the 2nd highest rate of primary and secondary syphilis among males of any age-group (36/100,000); whereas rates among males 15-19 yr old (8/100,000) are much lower. Female primary and secondary syphilis rates are much lower than male rates (5/100,000 among 20-24 yr olds; 3/100,000 among 15-19 yr olds) (see Chapter 245 ). Pelvic inflammatory disease (PID) rates are highest among females age 15-24 compared with older women.
Adolescents also carry a large burden of viral STIs. U.S. youth are at persistent risk for HIV infection (see Chapter 302 ). In 2015, youth age 13-24 yr accounted for 22% (8,807) of all new HIV diagnoses in the United States, with most (81%) occurring among gay and bisexual males. Of those new infections, 55% (4,881) were among blacks, 22% (1,957) among Hispanic/Latinos, and 17% (1,506) among whites. Only 10% of high school students have been tested for HIV. Among male students who had sexual contact with other males, only 21% have ever been tested for HIV.
Human papillomavirus (HPV) is the most frequently acquired STI in the United States. According to NHANES, prevalence of HPV vaccine types 6, 11, 16, and 18 (4vHPV ) declined between the prevacccine (2003–2006) and vaccine (2009–2012) eras: from 11.5% to 4.3% among females age 14-19 yr and from 18.5% to 12.1% among females age 20-24 (see Chapter 293 ).
Herpes simplex virus type 2 (HSV-2) is the most prevalent viral STI (see Chapter 279 ). NHANES data show that among 14-19 yr olds, HSV-2 seroprevalence has remained low (<2%, in 1999–2010 surveys). In addition, according to NHANES, HSV-1 seroprevalence among 14-19 yr olds has significantly decreased, from 39% in 1999–2004 to 30% in 2005–2010, indicating less orolabial infection in this age-group. Studies have also found that genital HSV-1 infections are increasing among young adults. Youth who lack HSV-1 antibodies at sexual debut are more susceptible to acquiring a genital HSV-1 infection and developing symptomatic disease from primary genital HSV-2 infection. Increasing oral sex among adolescents and young adults also has been suggested as a contributing factor in the rise in genital HSV-1 infections.
Pathogenesis
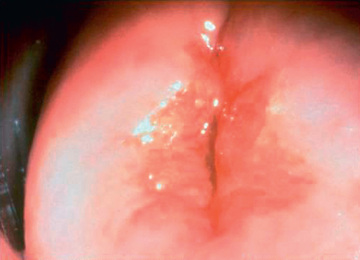
During puberty, increasing levels of estrogen cause the vaginal epithelium to thicken and cornify and the cellular glycogen content to rise, the latter causing the vaginal pH to fall. These changes increase the resistance of the vaginal epithelium to penetration by certain organisms (including Neisseria gonorrhoeae ) and increase the susceptibility to others (Candida albicans and Trichomonas ; see Chapter 310 ). The transformation of the vaginal cells leaves columnar cells on the ectocervix, forming a border of the 2 cell types on the ectocervix, known as the squamocolumnar junction. The appearance is referred to as ectopy (Fig. 146.3 ). With maturation, this tissue involutes. Prior to involution, it represents a unique vulnerability to infection for adolescent females. The association of early sexual debut and younger gynecologic age with increased risk of STIs supports this explanation of the pathogenesis of infection in young adolescents.
Screening
Early detection and treatment are primary STI control strategies. Some of the most common STIs in adolescents, including HPV, HSV, chlamydia, and gonorrhea, are usually asymptomatic and if undetected can be spread inadvertently by the infected host. Screening initiatives for chlamydial infections have demonstrated reductions in PID cases by up to 40%. Although federal and professional medical organizations recommend annual chlamydia screening for sexually active females <25 yr old, according to the National Center for Quality Assurance, in 2015 among sexually active 16-20 yr old females, approximately 42% of commercial health maintenance organization (HMO) members and 52% Medicaid HMO members were tested for chlamydia during the previous year. The lack of a dialog about STIs or the provision of STI services at annual preventive service visits to sexually experienced adolescents are missed opportunities for screening and education. Comprehensive, confidential, reproductive health services, including STI screening, should be offered to all sexually experienced adolescents (Table 146.2 ).
Common Infections and Clinical Manifestations
STI syndromes are generally characterized by the location of the manifestation (vaginitis) or the type of lesion (genital ulcer). Certain constellations of presenting symptoms suggest the inclusion of a possible STI in the differential diagnosis.
Urethritis
Urethritis is an STI syndrome characterized by inflammation of the urethra, usually caused by an infectious etiology. Urethritis may present with urethral discharge, dysuria, urethral irritation, or meatal pruritus. Urgency, frequency of urination, erythema of the urethral meatus, and urethral pain or burning are less common clinical presentations. Approximately 30–50% of males are asymptomatic but may have signs of discharge on diagnosis. On examination, the classic finding is mucoid or purulent discharge from the urethral meatus (Fig. 146.4 ). If no discharge is evident on exam, providers may attempt to express discharge by applying gentle pressure to the urethra from the base distally to the meatus 3-4 times. Chlamydia trachomatis and N. gonorrhoeae are the most commonly identified pathogens. Mycoplasma genitalium has been associated with urethritis, but data supporting Ureaplasma urealyticum have been inconsistent. Trichomonas vaginalis can cause nongonococcal urethritis (NGU), but the prevalence varies. HSV-1, HSV-2, and Epstein-Barr virus (EBV) are also potential urethritis pathogens in some cases. Sensitive diagnostic C. trachomatis and N. gonorrhoeae tests are available for the evaluation of urethritis. However, other pathogens can be considered when NGU is not responsive to treatment, although commercial diagnostic tests are not available for males. Noninfectious causes of urethritis include urethral trauma or foreign body. Unlike in females, urinary tract infections (UTIs) are rare in males who have no genitourinary medical history. In the typical sexually active adolescent male, dysuria and urethral discharge suggest the presence of an STI unless proven otherwise.

Epididymitis
The inflammation of the epididymis in adolescent males is most often associated with an STI, most frequently C. trachomatis or N. gonorrhoeae . The presentation of unilateral scrotal swelling and tenderness, often accompanied by a hydrocele and palpable swelling of the epididymis, associated with the history of urethral discharge, constitute the presumptive diagnosis of epididymitis. Males who practice insertive anal intercourse are also vulnerable to Escherichia coli infection. Testicular torsion , a surgical emergency usually presenting with sudden onset of severe testicular pain, should be considered in the differential diagnosis (see Chapter 560 ). The evaluation for epididymitis should include obtaining evidence of urethral inflammation by physical exam, Gram stain of urethral secretions, urine leukocyte esterase test, or urine microscopy. A C. trachomatis and N. gonorrhoeae nucleic acid amplification test (NAAT) should be performed.
Vaginitis
Vaginitis is a superficial infection of the vaginal mucosa frequently presenting as a vaginal discharge, with or without vulvar involvement (see Chapter 564 ). Bacterial vaginosis , vulvovaginal candidiasis , and trichomoniasis are the predominant infections associated with vaginal discharge. Bacterial vaginosis is replacement of the normal hydrogen peroxide (H2 O2 )–producing Lactobacillus species vaginal flora by an overgrowth of anaerobic microorganisms, as well as Gardnerella vaginalis, Ureaplasma , and Mycoplasma . Although bacterial vaginosis is not categorized as an STI, sexual activity is associated with increased frequency of vaginosis. Vulvovaginal candidiasis, usually caused by C. albicans , can trigger vulvar pruritus, pain, swelling, and redness and dysuria. Findings on vaginal examination include vulvar edema, fissures, excoriations, or thick curdy vaginal discharge. Trichomoniasis is caused by the protozoan T. vaginalis . Infected females may present with symptoms characterized by a diffuse, malodorous, yellow-green vaginal discharge with vulvar irritation or may be diagnosed by screening an asymptomatic patient. Cervicitis can sometimes cause a vaginal discharge. Laboratory confirmation is recommended because clinical presentations may vary and patients may be infected with >1 pathogen.
Cervicitis
The inflammatory process in cervicitis involves the deeper structures in the mucous membrane of the cervix uteri. Vaginal discharge can be a manifestation, but cervicitis frequently is asymptomatic, Patients also present with complaints of irregular or postcoital bleeding. Two major diagnostic signs characterize cervicitis: (1) a purulent or mucopurulent endocervical exudate visible in the endocervical canal or on an endocervical swab specimen (e.g., swab sign; Fig. 146.5 ), called mucopurulent cervicitis or cervicitis, and (2) sustained endocervical bleeding easily induced by gentle passage of a cotton swab through the cervical os, signifying friability. Cervical changes associated with cervicitis must be distinguished from cervical ectopy in the younger adolescent to avoid the overdiagnosis of inflammation (Fig. 146.6 ; see Fig. 146.3 ). The pathogens identified most frequently with cervicitis are C. trachomatis and N. gonorrhoeae, although no pathogen is identified in most cases. HSV is a less common pathogen associated with ulcerative and necrotic lesions on the cervix.


Pelvic Inflammatory Disease
PID encompasses a spectrum of inflammatory disorders of the female upper genital tract, including endometritis , salpingitis , tuboovarian abscess , and pelvic peritonitis , usually in combination rather than as separate entities. N. gonorrhoeae and C. trachomatis predominate as the involved pathogenic organisms in younger adolescents (see Chapters 219 and 253 ), although PID should be approached as multiorganism etiology, including pathogens such as anaerobes, G. vaginalis , Haemophilus influenzae , enteric gram-negative rods, and Streptococcus agalactiae. In addition, cytomegalovirus, Mycoplasma hominis , Ureaplasma urealyticum , and M. genitalium may be associated with PID. PID (tuboovarian abscess) has rarely been reported in virgins and is usually caused by E. coli and associated in some patients with obesity and possible pooling of urine in the vagina.
PID is difficult to diagnose because of the wide variation in the symptoms and signs. Many females with PID have subtle or mild symptoms, resulting in many unrecognized cases. Healthcare providers should consider the possibility of PID in young, sexually active females presenting with vaginal discharge or abdominal pain.
The clinical diagnosis of PID is based on the presence of at least 1 of the minimal criteria, either cervical motion tenderness, uterine tenderness, or adnexal tenderness, to increase the diagnostic sensitivity and reduce the likelihood of missed or delayed diagnosis. Providers should also consider that adolescents are the population in whom PID is typically diagnosed and thus should have a low threshold for initiating empirical treatment. In addition, the majority of females with PID have either mucopurulent cervical discharge or evidence of white blood cells (WBCs) on a microscopic evaluation of a vaginal fluid–saline preparation. If the cervical discharge appears normal and no WBCs are observed on the wet prep of vaginal fluid, the diagnosis of PID is unlikely, and alternative causes of pain should be investigated. Specific, but not always practical, criteria for PID include evidence of endometritis on biopsy, transvaginal sonography or MRI evidence of thickened, fluid-filled tubes, or Doppler evidence of tubal hyperemia or laparoscopic evidence of PID.
Genital Ulcer Syndromes
An ulcerative lesion in a mucosal area exposed to sexual contact is the unifying characteristic of infections associated with these syndromes. These lesions are most frequently seen on the penis and vulva but also occur on oral and rectal mucosa, depending on the adolescent's sexual practices. HSV and Treponema pallidum (syphilis) are the most common organisms associated with genital ulcer syndromes.
Genital herpes , the most common ulcerative STI among adolescents, is a chronic, lifelong viral infection. Two sexually transmitted HSV types have been identified, HSV-1 and HSV-2. The majority of cases of recurrent genital herpes are caused by HSV-2. However, among young women and MSM, an increasing proportion of anogenital herpes has been HSV-1. Most HSV-2–infected persons are unaware of their diagnosis because they experience mild or unrecognized infections but continue to shed virus intermittently in the genital tract. Therefore, most genital herpes infections are transmitted by asymptomatic persons who are unaware of their infection.
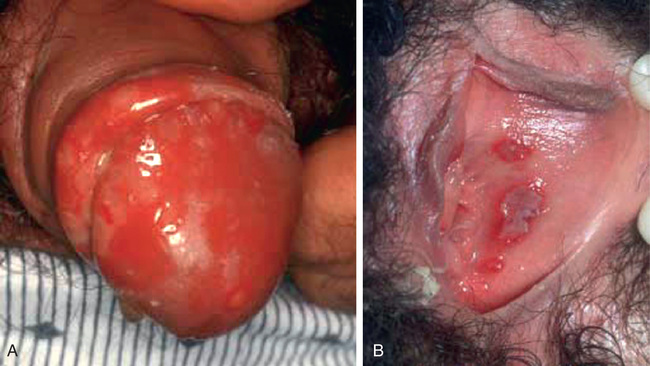
Although the initial herpetic lesion is a vesicle, by the time the patient presents clinically, the vesicle most often has ruptured spontaneously, leaving a shallow, painful ulcer (Fig. 146.7A ), although recurrences are generally less intense and painful (Fig. 146.7B ). Up to 50% of first genital herpes episodes are caused by HSV-1, but recurrences and subclinical shedding are much more frequent for genital HSV-2 infection.
Syphilis is a less common cause of genital ulcers in adolescents than in adults. Lymphogranuloma venereum caused by C. trachomatis serovars L1-L3 is uncommon, although outbreaks do occur in MSM. In these circumstances, proctitis or proctocolitis is the usual manifestation. HIV is often present in affected men. Unusual infectious causes of genital, anal, or perianal ulcers in the United States and other industrialized countries include chancroid and donovanosis.
Table 146.3 presents the clinical characteristics differentiating the lesions of the most common infections associated with genital ulcers, along with the required laboratory diagnosis to identify the causative agent accurately. The differential diagnosis includes Behçet disease (see Chapter 186 ), Crohn disease (Chapter 362 ), aphthous ulceration, and acute genital ulcers caused by cytomegalovirus (Chapter 282 ) or Epstein-Barr virus (Chapter 281 ). Acute genital ulcers often follow a flu or mononucleosis-like illness in an immunocompetent female and is unrelated to sexual activity. The lesions are 0.5-2.5 cm in size, bilateral, symmetric, multiple, painful, and necrotic, and are associated with inguinal lymphadenopathy. This primary infection is also associated with fever and malaise. The diagnosis may require Epstein-Barr virus titers, or polymerase chain reaction (PCR) testing. Treatment is supportive care including pain management.
Table 146.3
Signs, Symptoms, and Presumptive and Definitive Diagnoses of Genital Ulcers
| SIGNS/SYMPTOMS | HERPES SIMPLEX VIRUS | SYPHILIS (PRIMARY) | CHANCROID |
|---|---|---|---|
| Ulcers | Vesicles rupture to form shallow ulcers | Ulcer with well-demarcated indurated borders and a clean base (chancre) | Unindurated and undermined borders and a purulent base |
| Painful | Painful | Painless* | Painful |
| Number of lesions | Usually multiple | Usually single | Multiple |
| Inguinal lymphadenopathy | First-time infections may cause constitutional symptoms and lymphadenopathy. | Usually mild and minimally tender |
Unilateral or bilateral painful adenopathy in >50% Inguinal bubo formation and rupture may occur. |
| Clinical suspicion | Typical lesions; positive HSV-2 type-specific serology test | Early syphilis: typical chancre plus reactive nontreponemal test (RPR, VDRL) and no history of syphilis, or 4-fold increase in quantitative nontreponemal test in person with history of syphilis; positive treponemal EIA with reactive nontreponemal test (RPR, VDRL) and no prior history of syphilis treatment | Exclusion of other causes of ulcers in the presence of (a) typical ulcers and lymphadenopathy, (b) typical Gram stain, and (c) history of contact with high-risk individual (prostitute) or living in an endemic area |
| Definitive diagnosis | Detection of HSV by culture or PCR from ulcer scraping or aspiration of vesicle fluid | Identification of Treponema pallidum from a chancre or lymph node aspirate on dark-field microscopy | Detection of Haemophilus ducreyi by culture |
* Primary syphilitic ulcers may be painful if they become co-infected with bacteria or 1 of the other organisms responsible for genital ulcers.
DFA, Direct fluorescent antibody; EIA, enzyme immunoassay; HSV, herpes simplex virus; PCR, polymerase chain reaction; RPR, rapid plasma reagin; VDRL, Venereal Disease Research Laboratories.
Data from Centers for Disease Control and Prevention: Sexually transmitted diseases: treatment guidelines, MMWR 64(RR-3), 2015. https://www.cdc.gov/std/tg2015/default.htm .
Genital Lesions and Ectoparasites
Lesions that present as outgrowths on the surface of the epithelium and other limited epidermal lesions are included under this categorization of syndromes. HPV can cause genital warts and genital-cervical abnormalities that can lead to cancer (see Chapter 293 ). Genital HPV types are classified according to their association with cervical cancer. Infections with low-risk types, such as HPV types 6 and 11 , can cause benign or low-grade changes in cells of the cervix, genital warts, and recurrent respiratory papillomatosis. High-risk HPV types can cause cervical, anal, vulvar, vaginal, and head and neck cancers. High-risk HPV types 16 and 18 are detected in approximately 70% of cervical cancers . Persistent infection increases the risk of cervical cancer. Molluscum contagiosum and condyloma latum associated with secondary syphilis complete the classification of genital lesion syndromes.
As a result of the close physical contact during sexual contact, common ectoparasitic infestations of the pubic area occur as pediculosis pubis or the papular lesions of scabies (see Chapter 688 ).
HIV Disease and Hepatitis B
HIV and hepatitis B virus (HBV) present as asymptomatic, unexpected occurrences in most infected adolescents. High vaccination coverage rates among infants and adolescents have resulted in substantial declines in acute HBV incidence among U.S.-born adolescents. Risk factors identified in the history or routine screening during prenatal care are much more likely to result in suspicion of infection, leading to the appropriate laboratory screening, than are clinical manifestations in this age-group (see Chapters 302 and 385 ).
Diagnosis
Most often, adolescents infected with viral and bacterial STI pathogens do not report symptoms suggestive of infection. With the use of very sensitive, noninvasive chlamydia and gonorrhea NAAT, providers are finding that most genital infections in females as well as many males are asymptomatic. A thorough sexual history is key to identifying adolescents who should be screened for STIs and for identifying those who require a laboratory diagnostic evaluation for an STI syndrome.
When eliciting a sexual health history, discussions should be appropriate for the patient's developmental level. In addition to questions regarding vaginal or urethral discharge, genital lesions, and lower abdominal pain among females, one should ask about prior treatment of any STI symptoms, including self-treatment using nonprescription medications. Dyspareunia is a consistent symptom in adolescents with PID . Providers must ask about oral or anal sexual activity to determine sites for specimen collection.
Urethritis should be objectively documented by evidence of inflammation or infectious etiology. Patient complaint without objective clinical or laboratory evidence does not fulfill diagnostic criteria. Inflammation can be documented by (a) observing urethral mucopurulent discharge, (b) ≥2 WBCs per high-power field on microscopic examination of Gram stain urethral secretions, (c) urine microscopic findings of ≥10 WBCs per high-power field of first-void urine specimen, or (d) a positive urine leukocyte esterase test of a first-void specimen. Laboratory evaluation is essential to identify the involved pathogens to determine treatment, partner notification, and disease control. C. trachomatis and N. gonorrhoeae NAATs of a urine specimen are recommended. The presence of gram-negative intracellular diplococci on microscopy obtained from a male urethral specimen confirms the diagnosis of gonococcal urethritis.
An essential component of the diagnostic evaluation of vaginal, cervical, or urethral discharge is a chlamydia and gonorrhea NAAT. NAATs are the most sensitive chlamydia and gonorrhea tests available and are licensed for use with urine, urethral, vaginal, and cervical specimens. Many of the chlamydia NAATs are approved by the U.S. Food and Drug Administration (FDA) to test patient-collected vaginal swabs in the clinical setting and liquid cytology specimens. Female vaginal swab specimens and male first-void urine are considered the optimal specimen types. Female urine remains an acceptable chlamydia and gonorrhea NAAT specimen, but may have slightly reduced performance when compared with cervical or vaginal swab specimens. Urine is the recommended specimen for male urethral infection. Gonorrhea and chlamydia NAATs perform well on rectal and oropharyngeal specimens and can be performed by clinical laboratories that have completed the appropriate verification studies to obtain Clinical Laboratory Improvement Amendments (CLIA) approval, which includes most clinical laboratories.
Evaluation of adolescent females with vaginitis includes laboratory data. Traditionally, the cause of vaginal symptoms was determined by pH and microscopic examination of the discharge. However, CLIA-waived point-of-care vaginitis tests are available. Using pH paper, an elevated pH (i.e., >4.5) is common with bacterial vaginosis or trichomoniasis. Because pH testing is not highly specific, discharge should be further examined. For microscopic exam, a slide can be made with the discharge diluted in 1-2 drops of 0.9% normal saline solution and another slide with discharge diluted in 10% potassium hydroxide (KOH) solution. Examining the saline specimen slide under a microscope may reveal motile or dead T. vaginalis or clue cells (epithelial cells with borders obscured by small bacteria), which are characteristic of bacterial vaginosis . WBCs without evidence of trichomonads or yeast are usually suggestive of cervicitis. The yeast or pseudohyphae of Candida species are more easily identified in the KOH specimen (Fig. 146.8 ). The sensitivity of microscopy is approximately 50% and requires immediate evaluation of the slide for optimal results. Therefore, lack of findings does not eliminate the possibility of infection. More sensitive point-of-care vaginitis tests include the OSOM Trichomonas Rapid Test (Sekisui Diagnostics, Lexington, MA), an immunochromatographic capillary flow dipstick technology with reported 83% sensitivity. The OSOM BVBLUE Test (Sekisui) detects elevated vaginal fluid sialidase activity, an enzyme produced by bacterial pathogens associated with bacterial vaginosis, including Gardnerella , Bacteroides , Prevotella, and Mobiluncus , and has a reported 90% sensitivity. Both tests are CLIA waived, with results available in 10 min.

Clinical laboratory–based vaginitis tests are also available. The Affirm VPIII (Becton Dickenson, San Jose, CA) is a moderate-complexity nucleic acid probe test that evaluates for T. vaginalis , G. vaginalis , and C. albicans and has a sensitivity of 63% and specificity >99.9%, with results available in 45 min. Some gonorrhea and chlamydia NAATs also offer an assay for T. vaginalis testing of female specimens tested for N. gonorrhoeae and C. trachomatis , considered the gold standard for Trichomonas testing.
Objective signs of vulvar inflammation in the absence of vaginal pathogens, along with a minimal amount of discharge, suggest the possibility of mechanical, chemical, allergic, or other noninfectious irritation of the vulva (Table 146.4 ).
Table 146.4
| INFECTIVE DISCHARGE | OTHER REASONS FOR DISCHARGE |
|---|---|
| COMMON CAUSES | COMMON CAUSES |
| Organisms | |
| Conditions | |
| LESS COMMON CAUSES | |
| LESS COMMON CAUSES | |
From Mitchell H: Vaginal discharge—causes, diagnosis, and treatment, BMJ 328:1306–1308, 2004.
The definitive diagnosis of PID is difficult based on clinical findings alone. Clinical diagnosis is imprecise, and no single historical, physical, or laboratory finding is both sensitive and specific for the diagnosis of acute PID. Clinical criteria have a positive predictive value of only 65–90% compared with laparoscopy. Although healthcare providers should maintain a low threshold for the diagnosis of PID, additional criteria to enhance specificity of diagnosis, such as transvaginal ultrasonography, can be considered (Table 146.5 ).
Cell culture and polymerase chain reaction (PCR) are the preferred HSV tests . Viral culture sensitivity is low, and intermittent viral shedding causes false-negative results. NAATs, including PCR assays for HSV DNA, are more sensitive and increasingly available for diagnosing genital HSV. The Tzanck test is insensitive and nonspecific and should not be considered reliable.
Accurate type-specific HSV serologic assays are based on the HSV-specific glycoproteins G2 (HSV-2) and G1 (HSV-1). Both laboratory-based point-of-care tests are available. Because almost all HSV-2 infections are sexually acquired, the presence of type-specific HSV-2 antibody implies anogenital infection. The presence of HSV-1 antibody alone is more difficult to interpret because of the frequency of oral HSV infection acquired during childhood. Type-specific HSV serologic assays might be useful in the following scenarios: (1) recurrent genital symptoms or atypical symptoms with negative HSV cultures; (2) a clinical diagnosis of genital herpes without laboratory confirmation; and (3) a patient with a partner with genital herpes, especially if considering suppressive antiviral therapy to prevent transmission.
For syphilis testing , nontreponemal tests, such as the rapid plasma reagin (RPR) or Venereal Disease Research Laboratories (VDRL), and treponemal testing, such as fluorescent treponemal antibody absorbed tests, the T. pallidum passive particle agglutination (TP-PA) assay, and various enzyme and chemiluminescence immunoassays (EIA/CIA), are recommended. However, many clinical laboratories have adopted a reverse sequence of screening in which a treponemal EIA/CIA is performed first, followed by testing of reactive sera with a nontreponemal test (e.g., RPR). A positive treponemal EIA or CIA test can identify both previously treated and untreated or incompletely treated syphilis . False-positive results can occur, particularly among populations with low syphilis prevalence. Persons with a positive treponemal screening test should have a standard nontreponemal test with titer (RPR or VDRL) to guide patient management decisions. If EIA/CIA and RPR/VDRL results are discordant, the laboratory should perform a different treponemal test to confirm the results of the initial test. Patients with discordant serologic results by EIA/CIA and RPR/VDRL testing whose sera are reactive by TP-PA testing are considered to have past or present syphilis; if sera is TP-PA nonreactive, syphilis is unlikely (Fig. 146.9 ).

Rapid HIV testing with results available in 10-20 min can be useful when the likelihood of adolescents returning for their results is low. Point-of-care CLIA-waived tests for whole blood fingerstick and oral fluid specimen testing are available. Clinical studies have demonstrated that the rapid HIV test performance is comparable to those of EIAs. Because some reactive test results may be false positive, every reactive rapid test must be confirmed.
Treatment
See Part XVI for chapters on the treatment of specific microorganisms and Tables 146.6 to 146.8 . Treatment regimens using nonprescription products for candidal vaginitis and pediculosis reduce financial and access barriers to rapid treatment for adolescents, but potential risks for inappropriate self-treatment and complications from untreated more serious infections must be considered before using this approach. Minimizing noncompliance with treatment, notifying and treating the sexual partners, addressing prevention and contraceptive issues, offering available vaccines to prevent STIs, and making every effort to preserve fertility are additional physician responsibilities.
Table 146.6
IM, Intramuscularly; IV, intravenously; NAAT, nucleic acid amplification test.
Adapted for Centers for Disease Control and Prevention: Sexually transmitted diseases: treatment guidelines, MMWR 64(RR-3), 2015. https://www.cdc.gov/std/tg2015/default.htm .
Table 146.7
Adapted from Centers for Disease Control and Prevention: Sexually transmitted diseases: treatment guidelines, MMWR 64(RR-3), 2015. https://www.cdc.gov/std/tg2015/default.htm .
Table 146.8
Management Guidelines for Uncomplicated Genital Warts and Genital Herpes in Adolescents and Adults
| PATHOGEN | RECOMMENDED REGIMENS | ALTERNATIVE REGIMENS AND SPECIAL CONSIDERATIONS |
|---|---|---|
| HUMAN PAPILLOMAVIRUS (HPV) | ||
| External anogenital warts (penis, groin, scrotum, vulva, perineum, external anus, and perianus) |
Patient applied: Imiquimod 3.75% cream self-applied to warts at bedtime nightly for up to 16 wk; wash off after 6-10 hr or Imiquimod 3 5% cream self-applied to warts at bedtime 3 times weekly for up to 16 wk; wash off after 6-10 hr or Podofilox 0.5% solution or gel self-applied to warts twice daily for 3 consecutive days each wk followed by 4 days of no therapy. May be repeated for up to 4 cycles. or Sinecatechins 15% ointment self-applied 3 times daily for up to 16 wk. Do not wash off after use, and avoid genital, anal, and oral sexual contact while ointment is on skin. Provider-administered: Cryotherapy with liquid nitrogen or cryoprobe. Repeat applications every 1-2 wk. or Surgical removal either by electrocautery, tangential excision with scissors or scalpel, or by carbon dioxide (CO2 ) laser or Trichloroacetic acid (TCA) or bichloracetic acid (BCA) 80–90%; small amount applied only to warts and allowed to dry, when white “frosting” develops; can be repeated weekly. |
Provider administered: Podophyllin resin 10–25% in a compound tincture of benzoin applied to each wart and then allowed to air-dry; thoroughly wash after off 1-4 hr; can be repeated weekly. Systemic toxicity has been reported when podophyllin resin was applied to large areas of friable tissue and was not washed off within 4 hr. Many persons with external anal warts also have intraanal warts and might benefit from inspection of anal canal by digital examination, standard anoscopy, or high-resolution anoscopy. |
| Cervical warts |
Cryotherapy with liquid nitrogen or Surgical removal or TCA or BCA 80–90% solution Management should include consultation with a specialist. |
|
| Vaginal warts |
Cryotherapy with liquid nitrogen; avoid cryoprobe use. or Surgical removal or TCA or BCA 80–90%; small amount applied only to warts and allowed to dry, when white “frosting” develops; can be repeated weekly. |
|
| Urethral meatal warts |
Cryotherapy with liquid nitrogen or Surgical removal |
|
| Intraanal Warts |
Cryotherapy with liquid nitrogen or Surgical removal or TCA or BCA 80-90% applied to warts. A small amount should be applied only to warts and allowed to dry, at which time a white “frosting” develops. Can be repeated weekly |
Management of intraanal warts should include consultation with a specialist. |
| HERPES SIMPLEX VIRUS (HSV; GENITAL HERPES) | ||
| First clinical episode |
Treat for 7-10 days with 1 of the following: Acyclovir 400 mg orally 3 times daily Acyclovir 200 mg orally 5 times daily Valacyclovir 1 g orally twice daily Famciclovir 250 mg orally 3 times daily |
Consider extending treatment if healing is incomplete after 10 days of therapy |
| Episodic therapy for recurrences |
Treat with 1 of the following: Acyclovir 400 mg orally 3 times daily for 5 days Acyclovir 800 mg orally twice daily for 5 days Acyclovir 800 mg orally 3 times daily for 2 days Valacyclovir 500 mg orally twice daily for 3 days Valacyclovir 1,000 mg orally once daily for 5 days Famciclovir 125 mg orally twice daily for 5 days Famciclovir 1,000 mg orally twice daily for 1 day Famciclovir 500 mg orally once, then 250 mg twice daily for 2 days |
Effective episodic treatment of recurrences requires initiation of therapy within 1 day of lesion onset or during the prodrome that precedes some outbreaks. The patient should be provided with a supply or a prescription for the medication with instructions to initiate treatment immediately when symptoms begin. |
| Suppressive therapy to reduce frequency of recurrences |
Treat with 1 of the following: Acyclovir 400 mg orally twice daily Valacyclovir 500 mg orally once daily* or 1 g orally once daily Famciclovir 250 mg orally twice daily |
All patients should be counseled regarding suppressive therapy availability, regardless of number of outbreaks per year. Since the frequency of recurrent outbreaks diminishes over time in many patients, providers should periodically discuss the need to continue therapy. |
* Valacyclovir 500 mg once daily might be less effective than other valacyclovir or acyclovir dosing regimens in patients who have very frequent recurrences (i.e., ≥10 episodes per year).
Adapted from Centers for Disease Control and Prevention: Sexually transmitted diseases: treatment guidelines, MMWR 64(RR-3), 2015. https://www.cdc.gov/std/tg2015/default.htm .
Chlamydia- and gonorrhea-infected males and females should be retested approximately 3 mo after treatment, regardless of whether they believe that their sex partners were treated, or whenever persons next present for medical care in the 12 mo following initial treatment. Once an infection is diagnosed, partner evaluation, testing, and treatment are recommended for sexual contacts within 60 days of symptoms or diagnosis, or the most recent partner if sexual contact was >60 days, even if the partner is asymptomatic. Abstinence is recommended for at least 7 days after both patient and partner are treated. A test for pregnancy should be performed for all females with suspected PID because the test outcome will affect management. Repeat testing 3 mo after treatment is also recommended for Trichomonas infection.
Diagnosis and therapy are often carried out within the context of a confidential relationship between the physician and the patient. Therefore, the need to report certain STIs to health department authorities should be clarified at the outset. Health departments are Health Insurance Portability and Affordability Act (HIPAA) exempt and will not violate confidentiality. The health department's role is to ensure that treatment and case finding have been accomplished and that sexual partners have been notified of their STI exposure. Expedited partner therapy (EPT) , the clinical practice of treating sex partners of patients diagnosed with chlamydia or gonorrhea, by providing prescriptions or medications to the patient to take to the partner without the healthcare provider first examining the partner, is a strategy to reduce further transmission of infection. In randomized trials, EPT has reduced the rates of persistent or recurrent gonorrhea and chlamydia infection. Serious adverse reactions are rare with recommended chlamydia and gonorrhea treatment regimens, such as doxycycline, azithromycin, and cefixime. Transient gastrointestinal side effects are more common but rarely result in severe morbidity. Most states expressly permit EPT or may allow its practice. Resources for information regarding EPT and state laws are available at the Centers for Disease Control and Prevention website (http://www.cdc.gov/std/ept/ ).
Prevention
Healthcare providers should integrate sexuality education into clinical practice with children from early childhood through adolescence. Providers should counsel adolescents regarding sexual behaviors associated with risk of STI acquisition and should educate using evidence-based prevention strategies, which include a discussion of abstinence and other risk reduction strategies, such as consistent and correct condom use. The U.S. Preventive Services Task Force recommends high-intensity behavioral counseling to prevent STIs for all sexually active adolescents. The HPV vaccine (Gardasil 9) is recommended for 11 and 12 yr old males and females as routine immunization. Catch-up vaccination is recommended for females age 13-26 and for males age 13-21 who have not yet received or completed the vaccine series; males age 22 through 26 may be vaccinated.